GLP-1 drugs are now at the center of conversations about weight loss, diabetes, and mental health. As prescriptions climb around the world, people are asking how GLP-1 and mental health are connected, not just how many kilos they might lose.
These medicines, including semaglutide (Ozempic, Wegovy), tirzepatide (Mounjaro, Zepbound), and others, act on hormones in the gut, pancreas, and brain. That means they can influence appetite, blood sugar, reward circuits, and possibly mood and anxiety. This article explains how these drugs work, what current evidence says about anxiety, ADHD, and other mental health issues, and how to discuss them safely with your doctor.
GLP-1 Medications And Mental Health – Why Everyone Is Asking Now
GLP-1 medications started as treatments for type 2 diabetes but are now famous for helping people lose substantial weight. As millions of people use them for obesity and metabolic health, stories about mood shifts, anxiety, and emotional changes have spread on social media and in clinics. Some users feel calmer, more confident, and less obsessed with food, while others report feeling flat, anxious, or “not like themselves.” Regulators such as the EMA and the Australian TGA have reviewed safety data on suicidal thoughts and depression in GLP-1 users. Overall, they did not find strong proof that GLP-1 drugs cause suicidal behavior, but they still recommend close monitoring of mood and behavior.
How GLP-1 Drugs Became So Popular
GLP-1 receptor agonists became popular because they delivered results where many other weight-loss strategies failed. In clinical trials, higher-dose semaglutide and similar drugs produced average weight loss of around 10–20 percent in people with obesity, which is far more than older medications and lifestyle changes alone for many patients. At the same time, they improved blood sugar, blood pressure, and cholesterol, making them attractive to doctors focused on cardiometabolic risk. As success stories spread and celebrities hinted at using these “weight-loss injections,” demand jumped and waiting lists grew. This sudden rise in real-world use created a natural experiment in how GLP-1 and mental health interact outside tightly controlled trials.
Why Mental Health Questions Emerged
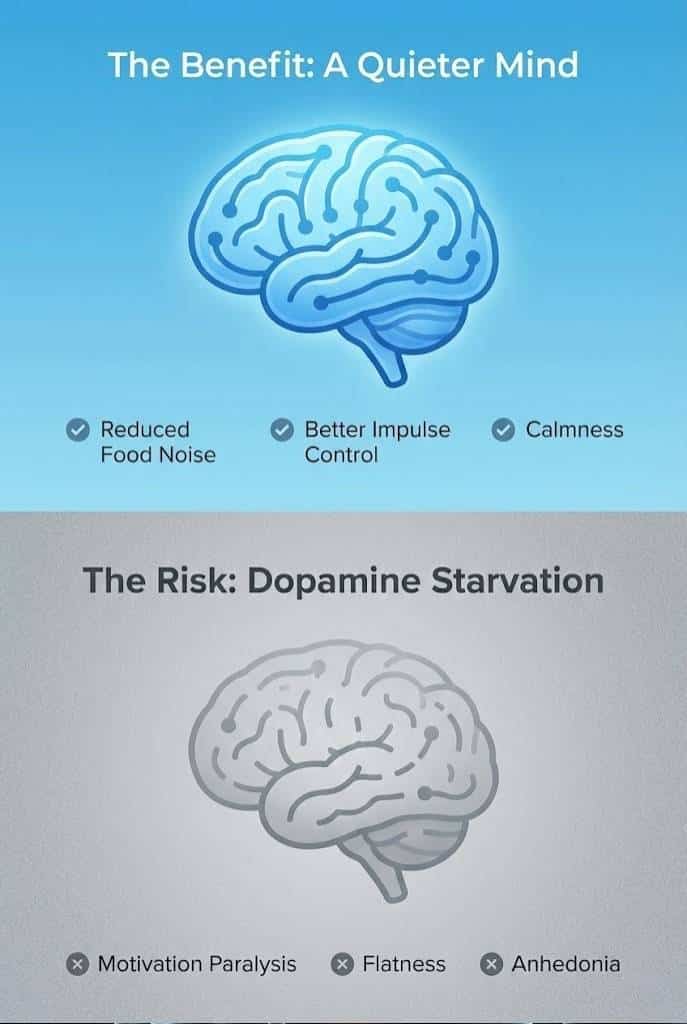
Mental health questions emerged because weight, self-image, and social reactions are deeply tied to how people feel. When weight changes quickly, relationships, confidence, and daily habits can shift just as fast. Some users say their minds feel quieter, with less “food noise” and fewer cravings, making it easier to focus on life and work. Others struggle with the identity shift that comes with rapid weight loss, fear of regaining weight, or guilt about needing medication in the first place. All of this happens alongside possible direct effects of GLP-1 drugs on brain circuits for reward and stress, which scientists now study more closely.
Regulator Reviews And Safety Alerts
In Europe, the EMA opened a review in 2023 after reports of suicidal thoughts and self-harm in people using GLP-1 drugs. Their later analysis in 2024 found no evidence that these medicines increase suicidal or self-injurious thoughts overall, but they urged continued monitoring because trials were not designed to measure rare psychiatric events. Australia’s TGA recently aligned warning labels across Ozempic, Wegovy, Saxenda, Trulicity, and Mounjaro, highlighting a potential risk of suicidal thoughts and advising patients to seek help if they notice mood or behavior changes. Media coverage of these alerts amplified concerns and made GLP-1 and mental health a mainstream topic.
What Patients And Doctors Want To Know
Patients now want clear answers about whether GLP-1 drugs will help or hurt their mental health, especially if they have anxiety, depression, ADHD, or a history of eating disorders. Doctors, on the other hand, must balance strong physical benefits against uncertain psychiatric risks, often with limited time and incomplete data. Both sides need simple, evidence-based explanations of the current science and honest discussion about what is still unknown. This article aims to support that conversation by summarizing key studies and highlighting practical points to cover in the clinic.
Why GLP-1 Mental Health Questions Are Rising
| Factor | What Is Happening | Why It Matters |
| Massive uptake | Millions use GLP-1 drugs for diabetes and obesity | Many more people notice mood and behavior changes |
| Social media and news | Stories highlight dramatic benefits and side effects | Shapes public hopes and fears |
| New mental health research | Studies assess mood, anxiety, and suicidality | Directly links GLP-1 and mental health outcomes |
| Regulator safety alerts | EMA and TGA review suicidal thoughts and depression reports | Doctors urged to monitor mental health closely |
GLP-1 Basics – How These Medications Work In The Body And Brain
To understand the link between GLP-1 and mental health, it helps to know how these drugs work in the body. GLP-1 (glucagon-like peptide-1) is a hormone released in the gut after we eat that signals fullness and helps manage blood sugar. GLP-1 receptor agonists mimic this hormone but last longer and act more strongly. They work on the pancreas, gut, and brain, which means they can influence both physical and emotional states. This wide action explains why some users report changes in energy, appetite, and mood during treatment.
What GLP-1 Receptor Agonists Are
GLP-1 receptor agonists are a class of injectable or oral drugs designed to activate GLP-1 receptors in the body. Common examples include semaglutide (Ozempic, Wegovy, Rybelsus), tirzepatide (Mounjaro, Zepbound, also a GIP agonist), liraglutide (Saxenda, Victoza), and dulaglutide (Trulicity). They were first approved for type 2 diabetes but later gained approval for chronic weight management in people with obesity or overweight plus risk factors. These medicines are usually taken once daily or once weekly, depending on the formulation, which helps with long-term adherence.
How GLP-1 Drugs Affect Blood Sugar And Weight
In the pancreas, GLP-1 drugs increase insulin when blood sugar is high and reduce glucagon, a hormone that raises blood sugar. This helps smooth out spikes and crashes in glucose, which can reduce fatigue, irritability, and other symptoms that sometimes feel like mood swings. In the gut, these medicines slow stomach emptying and increase feelings of fullness, so many people eat less without trying as hard to restrict. Over time, clinical trials show that higher-dose GLP-1 or dual agonist regimens can lead to 10–20 percent average weight loss, which is often enough to improve blood pressure, cholesterol, sleep apnea, and joint pain.
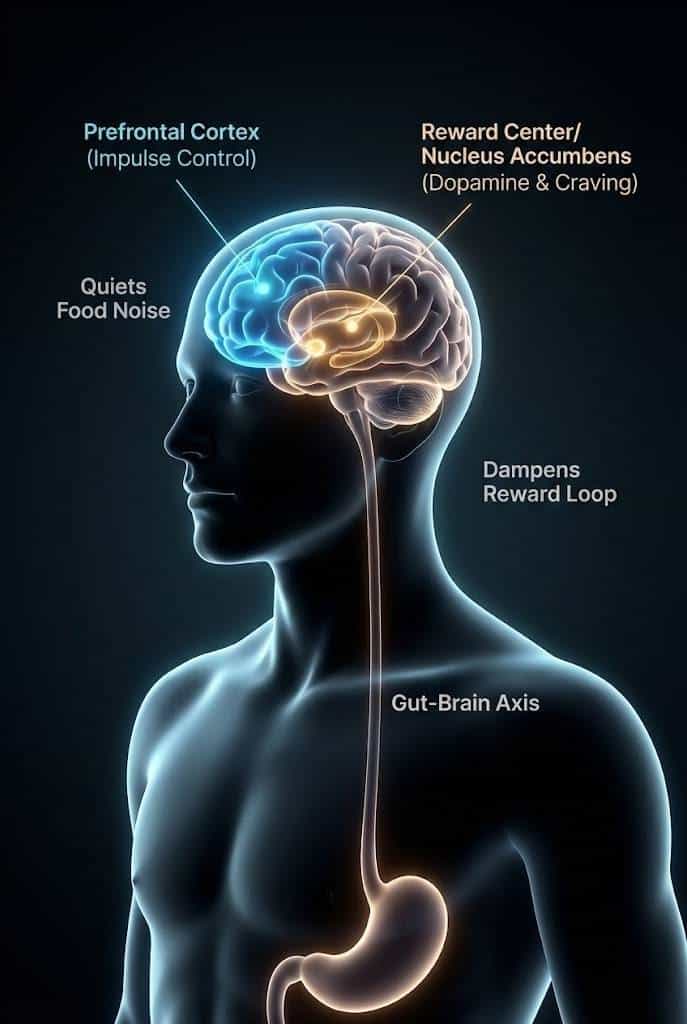
GLP-1 In The Brain And Mental Health Pathways
GLP-1 receptors are also found in brain regions that control appetite, reward, stress, and learning. Animal studies suggest that activating these receptors can alter dopamine signaling, reduce neuroinflammation, and influence fear and anxiety behaviors. These effects have led researchers to explore GLP-1 drugs as possible treatments or add-ons for conditions like depression, neurodegenerative disease, and substance use, although this work is still early. Because these pathways overlap with those involved in anxiety and ADHD, scientists are studying GLP-1 and mental health more carefully.
Why Body And Brain Effects Are Hard To Separate
For many patients, it is hard to tell whether mental changes come from the drug’s effects on the brain or from life changes caused by weight loss and better physical health. Improved blood sugar and weight can reduce pain, fatigue, and stigma, which naturally lifts mood in many people. At the same time, rapid weight loss and appetite changes can be stressful or destabilizing, especially if they interact with existing mental health conditions. This overlap makes it tricky to draw a clean line between direct and indirect effects of GLP-1 and mental health outcomes.
How GLP-1 Drugs Act In Body And Brain
| Site | Main Effect | Possible Mental Health Impact |
| Pancreas | More insulin, less glucagon | Fewer blood sugar swings and energy crashes |
| Gut | Slower stomach emptying, more fullness | Less binge eating and food preoccupation |
| Brain | Changes in reward, stress, inflammation | May alter mood, anxiety, motivation, and cognition |
| Weight | 10–20% loss in many trial participants | Better body image but also identity adjustments |
GLP-1 And Mental Health: What Research Shows So Far
Research on GLP-1 and mental health has grown quickly over the last few years. Studies now include randomized trials, observational databases, and systematic reviews. Overall, trials suggest that GLP-1 drugs do not cause large increases in depression or suicidal thoughts in most people. At the same time, safety reports and some observational work show signals for psychiatric side effects in a small number of users. The picture is mixed, but it leans toward modest effects that depend on each person’s history and context.
Findings From Randomized Clinical Trials
Randomized trials offer the clearest view of average effects. A major analysis in JAMA Internal Medicine pooled data from four semaglutide trials in people with overweight or obesity. It found no clinically meaningful differences in depression scores between semaglutide and placebo groups and similar rates of suicidal thoughts or behavior on both treatments. This supports the idea that GLP-1 drugs are psychiatrically neutral for many people without major mental illness at baseline.
Systematic Reviews And Meta-Analyses
A 2024 systematic review in Current Treatment Options in Psychiatry concluded that GLP-1 receptor agonists show potential neuroprotective and psychotropic effects, with tentative benefits for depression and anxiety in some patients, but also highlighted case reports of psychiatric adverse effects. A more recent 2025 review in a diabetes journal evaluated the psychiatric safety of GLP-1 drugs and found no strong evidence of increased suicidality, while still calling for better-designed studies focused on mental health outcomes. Together, these reviews point to GLP-1 and mental health as an area of emerging but still incomplete knowledge.
Observational Data And Safety Signals
Large health databases and adverse event reporting systems add another layer. Some observational analyses show that people on GLP-1 drugs may have equal or lower rates of new depression or suicidal ideation compared with those on other diabetes therapies, possibly because of improved physical health. On the other hand, pharmacovigilance analyses have detected more reports of depression, anxiety, suicidal thoughts, and eating disorders linked to some GLP-1 drugs, especially semaglutide, though these reports do not prove causation. These signals are important early warnings that inform regulator reviews and label changes.
Genetic studies, including Mendelian randomization research, look at lifelong differences in GLP-1 signaling and their association with mental illness risk. So far, they have not found strong direct links between GLP-1 pathways and most common psychiatric conditions, which suggests that any effect of GLP-1 and mental health is likely modest and highly context-dependent. Mechanistic lab work still shows that GLP-1 signaling can influence brain inflammation and neurotransmitters, but translating these findings into clear clinical predictions remains challenging.
Evidence Snapshot On GLP-1 And Mental Health
| Evidence Type | Main Finding | Key Message |
| Randomized clinical trials | No major increase in depression or suicidality vs placebo | GLP-1s look broadly psychiatrically safe on average |
| Systematic reviews | Mix of small benefits and some reported risks | Effects are modest and vary between individuals |
| Observational and safety data | Signals for depression, SI, eating disorders in some | Justifies careful monitoring, not panic |
| Genetic and mechanistic work | Weak direct link to most mental illnesses | Context and personal history matter a lot |
GLP-1 And Anxiety – Can These Medications Help Or Harm?
Anxiety is one of the most common mental health issues people ask about when starting GLP-1 therapy. For some, better blood sugar control and weight loss reduce everyday anxiety about health, eating, and social situations. For others, changes in appetite, body image, and physical sensations can make anxiety worse. The same drug class can therefore calm one person and unsettle another. Understanding how GLP-1 drugs interact with anxiety helps patients and doctors decide on the right pace and level of monitoring.
How GLP-1 Could Reduce Anxiety?
GLP-1 drugs can indirectly reduce anxiety by stabilizing blood sugar, which helps avoid jittery, irritable feelings associated with glucose swings. Weight loss may ease social anxiety about appearance, especially in cultures where weight stigma is strong. When food thoughts quiet down and binge episodes become less frequent, many people feel more in control of their eating, which can reduce guilt, shame, and worry. Improved sleep and physical fitness from better metabolic health also support an overall calmer nervous system.
How GLP-1 Could Trigger Or Worsen Anxiety?
On the other hand, GLP-1 drugs can provoke or worsen anxiety in some users. Dose increases may bring strong physical sensations such as nausea, palpitations, dizziness, or stomach discomfort, which can be misread as panic symptoms. Rapid weight loss may attract comments or expectations from others that feel stressful. Some people worry constantly about side effects, long-term safety, or the idea that they “need a shot to control eating,” which can fuel anticipatory anxiety. Because GLP-1 drugs affect brain stress circuits, they may also directly increase anxious feelings in a small subset of people.
What Studies Say About Anxiety Outcomes?
Clinical trials have not shown large increases in anxiety disorders among people taking GLP-1 drugs compared with placebo. Some analyses suggest neutral or slightly improved anxiety scores over time, likely tied to better physical health and quality of life. However, case reports and post-marketing data include individuals whose anxiety or panic symptoms seemed to start or worsen after beginning GLP-1 therapy or increasing doses. This dual picture supports the idea that GLP-1 and mental health interact in personalized ways rather than showing a simple “good” or “bad” effect.
Practical Steps To Manage Anxiety On GLP-1 Drugs
People with a history of anxiety can still use GLP-1 drugs, but they should do so with a clear plan. It helps to start low and titrate doses slowly, especially if you are sensitive to physical sensations. Keeping a simple log of sleep, appetite, and anxiety ratings during the first months can show patterns early. Working with a therapist or counselor at the same time adds support if worries increase. Most importantly, any sudden spikes in anxiety, panic, or intrusive thoughts should be discussed promptly with a healthcare professional rather than ignored.
GLP-1 And Anxiety – Potential Upsides And Downsides
| Aspect | Possible Helpful Effect | Possible Risk Or Challenge |
| Blood sugar control | Fewer “crash” feelings and irritability | Fear of hypoglycemia or side effects |
| Appetite and weight | Less food worry, improved body image | Pressure about weight loss or regain |
| Brain and stress | Calmer reward and stress responses in some | Heightened anxiety or restlessness in others |
| Life changes | Motivation to adopt healthier routines | Stress from rapid change and social reactions |
GLP-1 And ADHD – What We Know, What We Don’t
Many people with ADHD experience impulsive eating, emotional snacking, and difficulty with routine, which can contribute to weight gain. Because GLP-1 drugs reduce appetite and may dampen reward-driven eating, some wonder whether they might also improve ADHD symptoms. Current evidence suggests GLP-1 and mental health do interact in brain regions linked to attention and impulse control, but research is still too early to treat these drugs as ADHD medications. Understanding this nuance helps manage expectations.
Why ADHD And GLP-1 Are Connected In Discussion?
The link between ADHD and GLP-1 appears naturally because both involve reward pathways and self-control. People with ADHD often report craving quick comfort from food, struggling to plan meals, and overeating late at night. GLP-1 drugs blunt some of these drives by reducing hunger and making large meals uncomfortable. As a result, some users with ADHD report feeling more in control of their eating and daily routines, which may indirectly support better focus and stability.
Early Research On GLP-1 And Cognitive Function
Animal studies show that GLP-1 signaling can influence cognitive flexibility, learning, and impulsivity, and early human work explores GLP-1 drugs in conditions like Parkinson’s disease and dementia. These findings suggest GLP-1 pathways are relevant to brain health, but not specifically to ADHD. There are currently no large randomized trials targeting ADHD symptoms with GLP-1 treatment, so any claims of direct ADHD benefit remain speculative. Genetic studies also do not show a strong direct link between GLP-1 receptor pathways and ADHD risk.
Experience Of People With ADHD On GLP-1 Therapy
In real-world reports, some people with ADHD say GLP-1 treatment helps them feel less driven by food and more able to plan meals. Others describe brain fog, low motivation, or worsened sleep, which can make ADHD symptoms feel heavier. These mixed responses underline that GLP-1 and mental health interact differently from person to person. For someone whose weight dramatically impacts self-esteem and energy, physical benefits may improve day-to-day functioning; for others, side effects may complicate their existing challenges.
Using GLP-1 With ADHD Medication Safely
Many ADHD patients take stimulants like methylphenidate or amphetamines, or non-stimulants such as atomoxetine or guanfacine. These medicines can suppress appetite and affect blood pressure, just like GLP-1 drugs. Combining them can be safe under supervision, but it increases the need to watch nutrition, cardiovascular markers, and mood. Patients should never adjust stimulant doses on their own when they start a GLP-1 drug; any changes should be planned with their prescriber to avoid worsening attention, anxiety, or sleep.
GLP-1 And ADHD – Current Understanding
| Question | What Research Suggests | Practical Takeaway |
| Do GLP-1s treat core ADHD symptoms? | No strong human evidence yet | Not approved or recommended as ADHD meds |
| Can they help impulsive eating? | Often yes, in both ADHD and non-ADHD users | Useful for weight and metabolic goals |
| Are they safe with stimulants? | Limited data, no major red flags so far | Use only with medical supervision |
| How do they affect ADHD overall? | Effects on focus and motivation are mixed | Monitor carefully and adjust plans as needed |
Beyond Anxiety And ADHD – Other Mental Health Conditions And GLP-1s
GLP-1 and mental health are also linked through conditions like depression, eating disorders, and serious psychiatric illnesses. As GLP-1 drugs spread, scientists are exploring whether they might ease or worsen symptoms in these groups. Early evidence shows small mood benefits in some people and concerning side-effect reports in others. This makes careful screening and follow-up essential when mental illness is part of the picture.
Depression And Mood Symptoms
Several studies and reviews suggest that GLP-1 drugs may modestly improve depressive symptoms, likely through better physical health, reduced inflammation, and changes in reward processing. People who feel less pain, breathe more easily, and sleep better often report lighter mood and more motivation. In JAMA Internal Medicine analyses, semaglutide did not increase depressive symptoms or suicidal ideation compared with placebo, and small improvements in mood scores were observed in both groups. However, because people with severe depression are often excluded from trials, real-world responses can differ.
Eating Disorders And Body Image
Eating disorders add another layer of complexity. GLP-1 drugs aggressively reduce appetite and drive weight loss, which can be dangerous for people with anorexia, bulimia, or active binge eating disorder. They may be misused to push extreme restriction or may worsen body-image obsession when weight loss stalls or reverses. Some experts argue that GLP-1s should be avoided in active eating disorders unless used within a specialized team that includes mental health and nutrition professionals. Screening for past and current disordered eating is therefore crucial before prescribing.
Serious Mental Illness: Schizophrenia And Bipolar Disorder
In people with schizophrenia or bipolar disorder, antipsychotic medications often cause weight gain and metabolic problems. Small trials and reviews suggest GLP-1 drugs can help reverse some of this weight gain and improve metabolic risk, which may also positively affect quality of life and self-esteem. A 2025 analysis presented by the University of Bern highlighted mental health benefits and good tolerability of GLP-1 drugs in individuals with severe mental illness, though the sample sizes were still small. These findings are promising but must be balanced against complex medication regimens and higher baseline suicide risk in these populations.
The Need For Individualized Risk–Benefit Decisions
Because responses are so varied, clinicians must weigh GLP-1 and mental health effects on a case-by-case basis. A patient with severe obesity and mild, stable depression may gain far more than they risk by using a GLP-1 drug. Another patient with recent suicide attempts or active anorexia may face unacceptable dangers. Individualized decisions that consider diagnosis, past episodes, support systems, and alternative options are key to safe prescribing.
GLP-1s Across Different Mental Health Conditions
| Condition Type | Potential Benefits | Main Risks Or Concerns |
| Depression | Slight mood improvement in some people | Reports of depression and suicidal thoughts |
| Eating disorders | Appetite and weight reductions | Triggering or worsening disordered behaviors |
| Schizophrenia / bipolar | Reverses antipsychotic-related weight gain | Complex meds, higher baseline suicide risk |
| General stress / burnout | Better physical health and energy | Unrealistic expectations of a “magic fix” |
Who Might Benefit – And Who Should Be Extra Cautious?
Not everyone has the same balance of risks and benefits with GLP-1 therapy. Some people stand to gain a lot in both physical and mental health, while others may face more delicate trade-offs. Understanding how GLP-1 and mental health interact in different groups can guide safer choices. People with severe metabolic risk often benefit, but those with complex psychiatric histories need extra caution and tight follow-up.
Groups Likely To Benefit Overall
Adults with obesity and type 2 diabetes, especially those with heart disease or high cardiovascular risk, usually see strong physical improvements from GLP-1 therapy. Better blood sugar, blood pressure, and weight can reduce fatigue, pain, and daily stress, which often leads to improved mood and quality of life. People with long-standing distress about weight, who have tried many other approaches, may feel a sense of hope and control when GLP-1 drugs finally move the needle in a meaningful way.
Groups Who Need Extra Monitoring
People with a history of severe depression, bipolar disorder, psychosis, or suicide attempts should not automatically be excluded from GLP-1 therapy, but they do require more careful planning. Even small mood shifts can have larger consequences in these groups. Patients with current anorexia, bulimia, or active binge eating disorder also face higher risk because GLP-1 drugs can intensify restrictive behaviors or guilt around food. Teens and young adults may be especially vulnerable to identity and body-image changes. For all these groups, GLP-1 and mental health must be monitored together from day one.
Questions To Guide Risk–Benefit Decisions
Useful questions to ask in clinic include: What are my main physical risks if I do not use GLP-1 therapy? How stable is my mental health right now? What support systems do I have in place if things get harder? Are there non-drug alternatives or other medicines to try first? These questions help patients and clinicians see the full picture rather than focusing only on weight or short-term goals.
Role Of Support Networks
Family, friends, and mental health professionals can make GLP-1 use much safer for people with complex histories. Loved ones can notice changes in behavior or mood earlier than the patient or doctor. Therapists can help navigate body-image shifts, fear of regain, and pressure from others. When GLP-1 and mental health care are aligned and supported by a team, the chance of catching problems early is much higher.
Who May Benefit Versus Who Needs Extra Caution?
| Group | GLP-1 May Be Helpful When… | Extra Caution Or Alternatives When… |
| Adults with obesity and T2 diabetes | Strong physical benefits, stable mental health | Severe, unstable depression or recent suicidality |
| Emotional / binge eaters | No current severe eating disorder | Active anorexia, bulimia, or binge ED |
| Serious mental illness | Managed by psychiatry and a medical team | Poor follow-up or frequent crises |
| Teens and young adults | Under specialist obesity and mental health care | Limited psychological support or rapid changes |
How To Talk With Your Doctor About GLP-1 And Mental Health?
Because GLP-1 and mental health are so intertwined, good communication with your doctor is essential. Quick visits focused only on blood sugar or weight are not enough to manage the full impact of these drugs. You need time to share your history, goals, and worries. A structured conversation can turn GLP-1 therapy from a simple prescription into a shared plan that protects both body and mind.
Preparing For The Appointment
Before you see your doctor, write down all your current medications, including antidepressants, mood stabilizers, ADHD medicines, and supplements. Note any past mental health diagnoses, hospitalizations, or suicide attempts, even if they were years ago. Think about what you hope GLP-1 therapy will change beyond the number on the scale, such as energy, mobility, or confidence. Bringing notes helps you remember details when you are face to face with your clinician.
Questions To Ask During The Visit
During the appointment, ask your doctor to explain how GLP-1 and mental health might interact in your particular case. Good questions include: What are the benefits and risks for me given my history? How will we monitor my mood, anxiety, and sleep? What red-flag symptoms should I call you about immediately? Is there a plan if I do not tolerate the medicine or if my mental health worsens? These questions encourage shared decision-making instead of one-way advice.
Setting Up A Monitoring Plan
A clear monitoring plan reduces uncertainty. You might agree on check-ins every 4 to 12 weeks during dose titration, with extra visits if needed. Your doctor may use short questionnaires for depression or anxiety to track changes. You can use a simple daily or weekly log to note sleep, appetite, energy, and mood. This information helps decide whether GLP-1 therapy is supporting or harming your overall well-being.
When To Involve Mental Health Specialists?
If you have current or past serious mental illness, it often makes sense to involve a psychiatrist or psychologist before starting a GLP-1 drug. They can help anticipate potential problems, adjust existing medications, and support coping skills. Dietitians can also help you maintain adequate nutrition when appetite drops. Having a wider team does not mean GLP-1 therapy is unsafe; it means you are taking the full impact on your health seriously.
Discussion Checklist For Your Doctor Visit
| Topic | Questions To Ask | Why It Helps |
| History and goals | What from my past should we consider? | Focuses risk–benefit on your real situation |
| Benefits and risks | How do GLP-1 and mental health interact for me? | Links evidence to individual needs |
| Monitoring plan | How often will we check on mood and behavior? | Ensures early detection of problems |
| Backup plan | What if I want or need to stop the drug? | Reduces fear and helps you feel more in control |
What We Know, What We Don’t, And How To Stay Safe?
The relationship between GLP-1 and mental health is complex, but the evidence offers some clear messages. GLP-1 drugs are powerful tools for diabetes and obesity and, on average, do not appear to cause large increases in depression or suicidal thoughts compared with placebo. At the same time, real-world reports of psychiatric side effects, especially in vulnerable people, mean they are not risk-free. Safety depends heavily on individual history, support, and follow-up.
What The Evidence Says So Far?
Randomized trials and several systematic reviews suggest that GLP-1 drugs have a mostly neutral or slightly positive effect on mood and suicidality at the population level. Observational and pharmacovigilance data show that some people do experience depression, anxiety, or suicidal thoughts while on GLP-1 therapy, but these events are relatively rare and causality is hard to prove. Reviews by the EMA and TGA concluded that a direct link is not established, yet they recommended updating warnings and keeping a close watch. The best reading of the evidence is that GLP-1s are neither mental health cures nor clear psychiatric villains.
Practical Safety Principles For Patients
For patients, a few simple safety principles go a long way. Do not start or stop GLP-1 drugs or psychiatric medications on your own; always involve your prescriber. Track both physical and mental health changes, not just weight. Report new or worsening mood changes, anxiety, panic, or intrusive thoughts quickly rather than waiting for a routine visit. If you ever feel at risk of self-harm, seek emergency help or contact a crisis hotline immediately.
Practical Safety Principles For Clinicians
For clinicians, the key is to treat GLP-1 and mental health as linked domains rather than separate boxes. That means screening for psychiatric history before prescribing, discussing warning signs, and building a monitoring plan into the treatment. When patients have complex mental health histories, involving mental health professionals early can prevent crises later. Weighing benefits and risks over time rather than at a single point helps ensure that GLP-1 therapy remains a net positive.
The Road Ahead For Research
Future research will need to include more people with real-world psychiatric profiles, not just those without major mental illness. Better-designed trials and long-term observational studies can clarify which subgroups gain mental health benefits and which face more risk. As this evidence grows, guidelines will likely evolve to give more specific advice about GLP-1 and mental health for different conditions such as anxiety, ADHD, depression, and eating disorders.
Safety Snapshot For GLP-1 And Mental Health
| Area | Key Point | Action Step |
| Evidence | Trials suggest no major psychiatric harm overall | Use GLP-1s as one tool, not the only solution |
| Real-world reports | Some cases of depression, SI, eating problems | Take mental symptoms seriously and report early |
| Personal risk | Higher with severe mental illness or ED history | Use with close monitoring and support |
| Ongoing care | Requires regular check-ins and symptom tracking | Keep a simple log and stay in contact with your team |
Frequently Asked Questions (FAQs) About GLP-1s, Anxiety, ADHD, And Mental Health
People considering GLP-1 therapy often share the same questions about anxiety, depression, and focus. Clear answers based on current evidence can reduce fear and help them weigh their options. These FAQs summarize the most common concerns and link them back to what we know so far. They are not a substitute for medical advice, but they can guide better conversations with health professionals.
Can GLP-1 Medications Cause Anxiety Or Panic Attacks?
Some people do experience more anxiety or panic symptoms after starting or increasing a GLP-1 dose, especially if they are sensitive to physical sensations like nausea, palpitations, or dizziness. For others, better blood sugar control and reduced “food noise” actually lower anxiety, particularly around eating and social situations. Trials as a whole do not show a large increase in anxiety disorders compared with placebo, but individual susceptibilities matter. If new anxiety feels strong or worrying, it should be discussed with a clinician as soon as possible.
Do GLP-1 Drugs Increase Depression Or Suicidal Thoughts?
Randomized clinical trials and post hoc analyses of semaglutide find no meaningful difference in depression scores or suicidal ideation between GLP-1 and placebo groups. Regulators like the EMA and TGA have reviewed large amounts of data and concluded that a direct link to suicidal behavior is not proven, but they still updated labels to warn about possible mood changes. This means GLP-1 drugs do not appear to cause widespread depression or suicidality, but rare events may occur and should always be taken seriously.
Can GLP-1s Help With ADHD Symptoms Or Focus?
At this time, there is no solid human evidence that GLP-1 drugs reliably improve core ADHD symptoms such as inattention and hyperactivity. Some users with ADHD feel less impulsive around food and more able to stick to routines, which can indirectly support daily functioning. Others feel more tired or foggy, which can make ADHD harder to manage. GLP-1 drugs are not approved ADHD treatments, and they should not replace standard ADHD medications or behavioral therapies.
Is It Safe To Take GLP-1 Medications With ADHD Drugs Like Adderall Or Methylphenidate?
There are no large trials specifically studying the combination of GLP-1 drugs with ADHD stimulants, but both are used together in real-world practice. So far, no major safety signals have emerged, yet overlap in side effects such as appetite suppression, sleep changes, and cardiovascular effects means caution is needed. People using both should be monitored for weight loss, blood pressure, heart rate, and mood. Any unusual anxiety, insomnia, or mood swings should prompt a review of doses and timing.
What Should I Do If My Mood Or Anxiety Worsens On A GLP-1 Drug?
If you notice new or worsening depression, anxiety, panic, or suicidal thoughts after starting a GLP-1 medication, contact your prescriber as soon as possible. Do not stop the drug abruptly unless told to do so, as blood sugar and appetite can rebound. Your doctor may reduce the dose, change the titration schedule, involve a mental health specialist, or switch you to another therapy. If you feel at immediate risk of harming yourself, seek emergency help or call a crisis hotline right away.
FAQ Snapshot – GLP-1 And Mental Health
| Question | Short Answer |
| Can GLP-1s cause anxiety or panic? | Sometimes, especially around dose changes |
| Do they increase depression or suicide risk? | Trials say no; regulators still advise monitoring |
| Do they treat ADHD? | No, not approved and evidence is limited |
| What if my mood worsens? | Contact your doctor quickly; do not stop alone |
Takeaways
GLP-1 drugs are transforming treatment for obesity and type 2 diabetes, and they are now firmly linked to conversations about mental well-being. The best available evidence suggests that GLP-1 and mental health interact in nuanced ways. On average, these drugs do not appear to increase depression or suicidal ideation and may even support small mood gains for some, particularly as physical health improves. Yet real-world reports of anxiety, depression, disordered eating, and rare suicidal thoughts show that careful monitoring is essential, especially in people with prior mental illness.
For patients, the most important step is to treat GLP-1 therapy as a shared journey with healthcare providers, not a solo experiment. For clinicians, reviewing psychiatric history, setting up a monitoring plan, and involving mental health professionals when needed can make these powerful medications safer and more effective. When used thoughtfully, GLP-1 drugs can be part of a broader plan to support both physical health and mental resilience, rather than focusing on the scale alone.