For over 30 years, one man lived in the shadow of severe, treatment-resistant depression. His life was defined by endless hospitalizations, failed therapies, and repeated attempts to end his own suffering. Today, thanks to a groundbreaking personalized brain stimulation treatment, he has entered full remission and is experiencing something he hadn’t felt in decades—true joy.
This breakthrough has stunned psychiatrists and neuroscientists, who believe it could signal a new era in the fight against one of the world’s most disabling mental health conditions.
A Life Consumed by Depression
The participant, whose name has not been revealed to protect his privacy, was first hospitalized for depression at just 13 years old. From that moment, his adolescence and adulthood were consumed by a relentless cycle of mental illness.
- He underwent dozens of medications, sometimes in combination.
- He engaged in years of psychotherapy with little relief.
- He endured multiple hospitalizations as his condition spiraled out of control.
- He attempted suicide three times, convinced there was no way out of his despair.
By his early 40s, he had been living with treatment-resistant depression (TRD) for three decades. TRD is diagnosed when a patient fails to respond to at least two standard treatment attempts, such as antidepressants, therapy, or a combination of both. According to the National Institute of Mental Health (NIMH), TRD affects up to 30% of people with major depressive disorder, leaving millions worldwide without effective solutions.
Why Conventional Treatments Failed
When depression becomes resistant to standard care, psychiatrists often turn to more aggressive interventions. The most common is electroconvulsive therapy (ECT), a treatment that delivers small electric currents to the brain to induce controlled seizures.
- ECT can be effective for many patients, and it remains a standard option for severe or suicidal depression.
- However, it does not work for everyone.
- In this man’s case, he had already undergone three rounds of ECT. The first gave some temporary relief, but the second and third rounds offered no improvement at all.
One of the limitations of ECT is that it typically uses a standardized brain atlas, meaning doctors stimulate the same regions in every patient. But every brain is unique, and depression does not look the same from one individual to another. As neuroscientist Damien Fair from the University of Minnesota explained, it’s a “one-size-fits-all approach”—a serious limitation when treating a condition as complex as depression.
The Birth of a New Idea: Personalized Adaptive Cortical Electro-Stimulation (PACE)
This is where the new approach stands apart. Instead of stimulating the same region in every brain, researchers developed Personalized Adaptive Cortical Electro-stimulation (PACE).
Step 1: Mapping the Brain
The team used functional MRI (fMRI) to create a personalized brain map of the patient’s networks linked to depression. This revealed striking abnormalities:
- His salience network—the system that processes and prioritizes external stimuli—was nearly four times larger than normal.
- His default mode network (DMN)—which governs self-reflection and internal thoughts—was 25% smaller than in people without depression.
- His frontoparietal network, which helps with decision-making, was also abnormally small.
Such distortions in brain network structure may explain why traditional treatments never worked for him.
Step 2: Surgical Implantation
Surgeons implanted four clusters of electrodes over the borders of these networks. The electrodes were designed to send precise, weak electrical signals to specific regions.
Step 3: Testing and Adjustment
Researchers began testing the electrodes, stimulating each brain network individually to observe his reactions. What happened next stunned everyone.
Tears of Joy: A Rare Breakthrough in Psychiatry
The first time doctors stimulated his default mode network (DMN), something extraordinary happened.
He broke down in tears—not of despair, but of happiness. For the first time in over 30 years, he reported experiencing joy. According to psychiatrist Dr. Ziad Nahas, the study’s lead researcher, the patient said:
“I’m not sad. I’m just happy. I don’t know what to do with these emotions.”
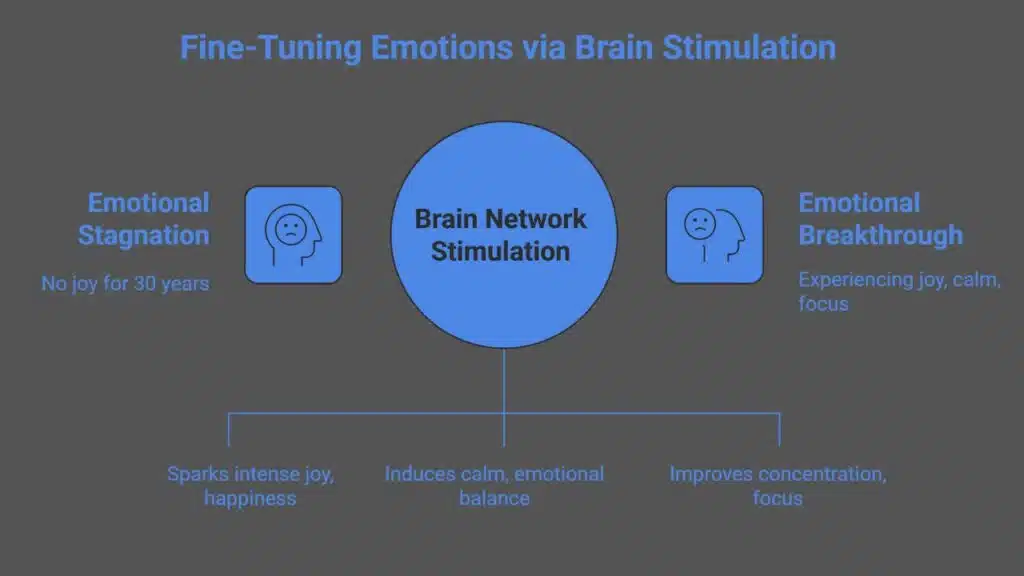
This was the beginning of a transformation. Different brain networks triggered different emotional outcomes:
- Default Mode Network (DMN): Sparked intense joy and happiness.
- Salience and Action-Mode Networks: Induced deep calm and emotional balance.
- Frontoparietal Network: Improved concentration and focus.
The team realized they had discovered a way to fine-tune emotions by stimulating specific brain networks.
The Recovery Timeline
The patient’s progress was carefully monitored over months, with stimulation sessions occurring daily:
- Every 5 minutes, a 1-minute electrical pulse was delivered to the electrodes.
- Researchers regularly adjusted settings using Bayesian statistical methods and patient feedback.
Here’s how his recovery unfolded:
| Time After Surgery | Outcome |
| 1–2 days | Experienced joy, calm, and improved focus during initial testing |
| 7 weeks | Suicidal thoughts completely disappeared |
| 6 months | Significant reduction in depression symptoms |
| 9 months | Full remission achieved |
| 24–30 months | Remission has been sustained for 2+ years |
By nine months, his depression had lifted entirely. For the first time in decades, he could live without constant darkness.
Living Again: A New Chapter
Recently, Dr. Nahas received an email from the participant. He was on a road trip with his family, enjoying life in a way he never thought possible. This was more than just a medical success—it was the restoration of a life once consumed by illness.
The patient’s case is still just one example, but for researchers, it represents a paradigm shift. As Dr. Nahas said:
“In psychiatry, we don’t have cures. But this is probably the closest we can get.”
Next Steps: Expanding the Research
The team has since implanted electrodes in a second participant and plans to include a third. Their long-term goal is to conduct a double-blind clinical trial to test whether this approach can work across larger groups of patients.
If successful, PACE could:
- Offer a new lifeline for people with treatment-resistant depression.
- Provide personalized treatment, unlike current methods.
- Open the door to treating other psychiatric conditions involving brain network dysfunction, such as anxiety or OCD.
Why This Matters
Depression is one of the leading causes of disability worldwide. According to the World Health Organization (WHO), more than 280 million people suffer from depression, and a significant percentage do not respond to existing treatments.
The success of PACE shows that mental illness does not have to mean permanent suffering. By harnessing modern brain-mapping technology, medicine can move beyond “trial-and-error” treatments and toward truly personalized care.
This story is not just about science—it’s about hope. After decades of despair, one man can now laugh, smile, travel with his family, and feel the simple joy of being alive.
The journey from darkness to light was made possible by a revolutionary personalized brain stimulation treatment. If future trials confirm these findings, psychiatry may soon enter a new age—one where precision brain therapies can restore lives once thought lost to depression.
The Information is Collected from New Scientist and and NPR.