By early 2026, the global mental health crisis has shifted decisively from being a private health concern to an acute societal issue. More than one billion people worldwide, that is nearly one-eighth of the global population, are living with a mental health condition. Issues once treated as individual failings are now recognized as structural challenges. Rapid technological change, prolonged economic uncertainty, and the steady erosion of social and community support systems have all played a role. Together, these forces have created a “silent emergency.” It is a crisis that increasingly threatens global productivity and social cohesion.
This moment did not arrive overnight. It has been decades in the making. In the early 2000s, mental health was a whispered subject. It was often left out of mainstream medical and policy conversations. Psychological distress was expected to be managed privately, hidden within families and personal lives. The mid-2010s marked a turning point. Digital-first living and algorithm-driven platforms began reshaping human interaction, attention, and self-worth. Social comparison became constant. Boundaries between work and rest blurred. Emotional fatigue intensified.
The COVID-19 pandemic acted as a catalyst, not the cause. Prolonged isolation, grief, job insecurity, and uncertainty pulled latent mental health struggles into public view. By 2024, loneliness was formally acknowledged by several national health agencies as a public health concern. Now, in 2026, the world is dealing with the aftershocks. Technological acceleration has far outpaced the human brain’s evolutionary capacity to cope with stress, isolation, and continuous performance pressure.
Why Mental Health Struggles Remain a Social Stigma
“I am going through severe mental trauma after breaking up with my girlfriend,” says Ankit Jha (name changed on request). “She rejected me because she is in love with someone she considers superior to me. Since then, I have begun to feel hopeless, as if I am of no use. I now have to convince my parents to allow me to see a counsellor, because seeking mental health support still carries a strong social stigma.”
Mental health issues remain stigmatized because emotional suffering is still widely misunderstood as a weakness rather than a legitimate health condition. In many societies, distress is expected to be absorbed silently, managed through endurance or denial rather than professional care. Vulnerability is seen as a failure of character, discouraging people from acknowledging pain even when it becomes overwhelming.
A key reason for this stigma is limited mental health literacy. Conditions such as depression, anxiety, and trauma often do not present visible symptoms. Their effects fluctuate, making them easier to dismiss as overthinking, lack of discipline, or temporary sadness. Families and communities frequently trivialize suffering, urging individuals to “adjust” instead of seek help.
Cultural expectations deepen this silence. In family-centric societies, mental health struggles are often viewed as reflections of poor upbringing or moral weakness, with fears that disclosure could damage marriage prospects, careers, or social standing. Gender norms compound the problem: men are conditioned to suppress emotion and equate vulnerability with failure, while women’s distress is frequently minimized or labelled as emotional excess.
Limited access to affordable mental health care further reinforces stigma. When treatment is scarce or expensive, seeking help appears extreme rather than routine, pushing people to delay intervention until their condition worsens.
Key Takeaways: The 2026 Mental Health Landscape (What the Data Shows So Far)
- Macroeconomic Toll: Depression and anxiety alone cost the global economy over $1 trillion annually, primarily through lost productivity, absenteeism, and reduced work performance.
- The Youth Crisis: Around one in seven adolescents aged 10–19 lives with a mental health condition, with suicide remaining among the leading causes of death in this age group.
- The Treatment Gap: In low-income countries, treatment gaps frequently exceed 50–75%, while even high-income nations face gaps of nearly 50% due to shortages of trained professionals.
- Digital Coping Shift: Millions of adults are turning to AI-powered tools, mental health apps, and conversational platforms for emotional support, reflecting unmet demand in traditional care systems.
- Burnout Threshold: A majority of global employees now report symptoms of burnout, forcing employers to treat mental well-being as a core productivity and retention issue.
The Macroeconomic Drain: Why GDP and Mental Health Are Inseparable
In 2026, the economic cost of mental ill-health is no longer hidden. Global institutions increasingly recognize psychological well-being as a foundational driver of labour participation and economic resilience. Depression and anxiety alone account for an estimated 12 billion working days lost each year worldwide.
This loss extends beyond absenteeism to “presenteeism,” where individuals remain at work but function far below capacity due to emotional exhaustion and cognitive overload. The cumulative impact on innovation, efficiency, and decision-making is profound. For the first time, corporate risk frameworks are beginning to list psychosocial risk alongside inflation, labour shortages, and supply-chain disruptions.
Mental health is no longer a peripheral social issue. It has become a defining economic, cultural, and public health challenge of this decade, one that demands structural solutions rather than silence.
Estimated Global Economic Impact of Mental Health (Synthesized Models, 2020–2026)
| Year | Total Global Cost (Trillions USD) | Productivity Loss (Annual) | Avg. Govt Health Spend on MH |
| 2020 | $2.5 T | $0.6 T | 1.9% |
| 2022 | $3.1 T | $0.8 T | 2.0% |
| 2024 | $4.2 T | $0.9 T | 2.1% |
| 2026 (Est) | $5.0 T | $1.1 T | 2.2% |
*Figures are indicative estimates synthesized from WHO, World Economic Forum, OECD, and World Bank modelling, intended to illustrate trend direction rather than precise year-by-year totals.
While the World Health Organization estimates that depression and anxiety alone cost the global economy over $1 trillion annually in lost productivity, broader economic models that account for disability, healthcare burden, workforce attrition, and indirect social costs place the total economic impact of mental health conditions in the multi-trillion-dollar range.
The data suggest that although government spending on mental health is gradually increasing, it is not keeping pace with the scale of economic loss. In several sectors, businesses that fail to address employee wellbeing report sharply rising turnover and attrition costs compared to pre-2020 levels, as workers increasingly seek environments that prioritize psychological safety.
The Digital Architecture of the Mental Health Crisis
The “why” of this crisis is deeply rooted in our digital environment. In 2026, we are witnessing the cumulative results of a decade-long experiment in hyper-connectivity. The “always-on” culture has steadily eroded the boundaries between work and rest, creating a state of continuous mental engagement. Neurologists and cognitive scientists increasingly describe this condition as cognitive overload, where the brain is forced to process far more information than it evolved to handle.
Digital platforms built around constant alerts, rapid feedback loops, and uninterrupted scrolling have altered how attention functions. Algorithms designed to maximize “time on site” repeatedly stimulate the brain’s reward circuitry, reinforcing compulsive engagement. While these mechanisms generate short-term gratification, researchers warn that sustained exposure may disrupt emotional regulation, increase stress hormones, and contribute to anxiety and depressive symptoms over time. The issue is less about a single chemical imbalance and more about chronic neurological strain caused by relentless stimulation.
Among young people, the psychological consequences are particularly pronounced. The gap between “filtered reality” and lived experience has widened dramatically. Curated images of success, beauty, and happiness dominate screens, creating unrealistic benchmarks against which everyday life is measured. This persistent comparison fosters feelings of inadequacy, low self-worth, and social anxiety, especially during formative years when identity and self-esteem are still developing.
At the same time, the rise of AI-driven interactions has introduced a new paradox of connection. Chatbots, recommendation engines, and automated social responses offer instant engagement without emotional risk. While these tools provide convenience and companionship, they often lack the depth, reciprocity, and unpredictability of human relationships. The result is what psychologists describe as pseudo-connection, a state in which individuals are constantly engaged yet emotionally unfulfilled.
This architecture of digital life has not created anxiety in isolation, but it has amplified existing vulnerabilities. In a world of constant connectivity, silence feels uncomfortable, disconnection feels like failure, and rest is mistaken for unproductivity. Modern anxiety, increasingly, is not just a personal condition, it is a byproduct of the systems we inhabit daily.
Says psychiatrist Dr. Sanjay Chugh, “It is incorrect to say that mental health is becoming a crisis. It was always a crisis. What has changed is recognition. Today, an estimated 40–50% of people live with some condition linked to brain functioning. These issues may appear as physical illnesses, affecting the stomach, lungs, skin, or heart. But either their roots lie in the brain, or brain processes worsen them. The numbers are so large that no other organ system comes close in disease prevalence. This is now an emergency because of its sheer scale. The first step toward control is awareness at the grassroots level.”
Adds Dr Chugh, “Psychiatric and psychological problems are real, scientific conditions. Misconceptions like ‘it will go away on its own’ only make them chronic. There is nothing socially unacceptable about mental illness, and seeking professional help must be normalized.”
Psychiatrist Dr Sanjay Chugh discusses the mental health crisis in this audio.
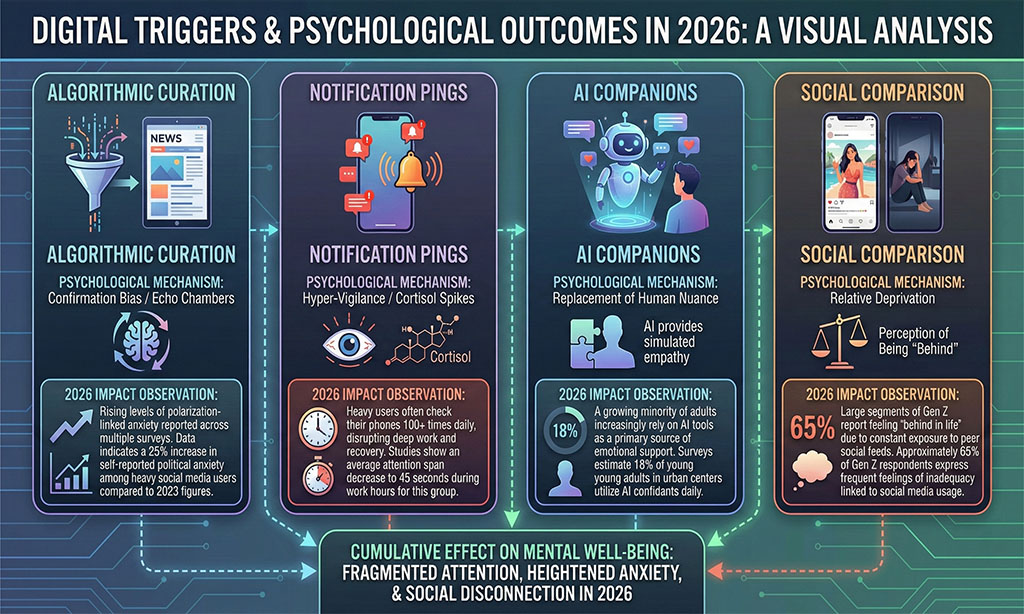
Digital Triggers and Psychological Outcomes in 2026
| Technology Element | Psychological Mechanism | 2026 Impact Observation |
| Algorithmic Curation | Confirmation Bias / Echo Chambers | Rising levels of polarization-linked anxiety reported across multiple surveys. |
| Notification Pings | Hyper-Vigilance / Cortisol Spikes | Heavy users often check their phones 100+ times daily, disrupting deep work and recovery. |
| AI Companions | Replacement of Human Nuance | A growing minority of adults increasingly rely on AI tools as a primary source of emotional support. |
| Social Comparison | Relative Deprivation | Large segments of Gen Z report feeling “behind in life” due to constant exposure to peer social feeds. |
These observations synthesize findings from multiple global surveys, platform-usage studies, and academic research and should be read as directional indicators rather than precise population measurements.
This digital architecture is particularly damaging because it is pervasive. Unlike traditional stressors, digital stress follows the individual into their private sanctuary, their home, leaving no room for recovery.
The Treatment Gap: A Tale of Two Worlds
As of January 2026, the disparity in mental health resources has become a significant geopolitical issue. High-income nations like the US and Germany are investing heavily in “Mental Health Tech,” with a market valued at over $9 billion, while low-to-middle-income countries continue to struggle with a severe shortage of trained personnel.
In India, for example, the Indian Psychiatric Society reports that nearly 80–85% of individuals suffering from psychiatric disorders do not receive timely care. This is due both to a shortage of professionals and persistent social stigma that delays help-seeking until crises occur.
Resource Allocation: High-Income vs. Low-Income (2026 Status)
| Resource Indicator | High-Income (Avg.) | Low-Income (Avg.) |
| Mental Health Budget/Person | $65.00 | $0.04 |
| Specialists per 100,000 People | 50.2 | 1.3 |
| Access to Digital Teletherapy | 72% | <10% |
| Treatment Gap (Untreated Cases) | 48% | 88% |
Figures reflect synthesized estimates from WHO, World Bank, and national mental health surveys and should be interpreted as indicative ranges rather than exact country-level measurements.
This treatment gap creates a vicious cycle: untreated mental illness leads to disability, which contributes to poverty, further worsening mental health conditions. Experts warn that without a global “knowledge transfer” of mental health tools and strategies, the Global South could face a massive labor crisis by 2030.
Workplace Transformation and the “Burnout Ceiling”
“I wake up every morning dreading going to the office, but there is no way out,” says Puja Deshpande (name changed on request). “As a single woman, I have to earn a living, regardless of how frightened or exhausted I feel.”
The workplace has become a primary stage for the mental health crisis. In 2026, the concept of a “safe and healthy working environment” has expanded to include psychological safety, yet implementation remains inconsistent across sectors. Surveys show widespread burnout and stress: many workers report negative mental health impacts from job demands, with large portions of the workforce saying they have considered leaving due to mental health concerns.
Mental health‑related absences are also rising, and a majority of employees feel their employers do not provide sufficient support or space to openly discuss psychological struggles without fear of judgment or professional repercussions.
Comparative Industry Stress & Burnout Analysis (2026 Data)
| Industry Sector | Common Stress/Burnout Issues Reported |
| Healthcare & Social Care | High emotional labor burden: Workers face constant compassion fatigue, understaffing, and moral injury, frequently ranking as the leading category for clinical burnout. |
| Education & Research | Workload pressure & emotional strain: Educators cite overwhelming administrative duties, student behavioral challenges, and lack of dedicated mental health support as primary stressors. |
| Construction & Engineering | Physical demand & stigma: A high-risk environment where physically grueling work is coupled with a strong cultural stigma that prevents workers from reporting psychological distress. |
| Tech & Professional Services | Long hours & high expectations: An “always-on” culture driven by tight deadlines, performance metrics, and increasing anxiety regarding AI-driven job displacement. |
These qualitative trends are recognized in multiple workplace mental health surveys rather than precise percentages.
A concerning dynamic is that many employees avoid reporting mental health issues, opting to use regular leave to manage stress and burnout due to fear of stigma or negative repercussions at work, a behavior noted in workplace wellbeing research.
The Rise of the “Off-Label” AI Therapist
One of the most significant shifts in 2026 is the democratization, and risks of AI in mental health. Because human therapists are expensive and often have months-long waiting lists, millions are turning to AI.
Generative AI models are now being used “off-label” for emotional support. While these tools provide immediate, 24/7, and stigma-free interaction, they lack clinical validation. In early 2026, the industry is at a crossroads: do we embrace AI as a necessary triage tool, or do we regulate it to prevent “hallucinated” advice that could endanger lives?
The AI Mental Health Market Shift
The global AI in mental health market is projected to be in the multi-billion-dollar range by 2026, with several market research reports estimating it around $1.7–$2 billion and forecasting robust growth (over 20% CAGR through the early 2030s). Adoption of artificial intelligence tools for emotional support and self-help is rising rapidly, with surveys indicating that a substantial share of digitally literate adults have experimented with large language models and related apps for psychological support. However, most of this usage occurs on general-purpose platforms rather than dedicated clinical products, raising questions about quality and safety.
Expert Perspectives: The Medicalization Debate
There is a growing intellectual rift among experts in 2026. On one side, clinical psychologists emphasize the need for better screening and early intervention (the “Medical Model”). They cite that 50% of disorders start by age 14, meaning school-based intervention is the most effective way to save the next generation.
On the other side, “Social Model” advocates argue that we are over-medicalizing human suffering. They suggest that the “crisis” is a rational reaction to an irrational world, climate anxiety, political polarization, and economic precariousness. They argue that “prescribing a pill or a chatbot” for a person who cannot afford rent is a failure of social policy, not a victory for medicine.
“The crisis is not just inside our heads; it’s in our neighborhoods, our screens, and our bank accounts. We cannot treat our way out of a societal collapse of community.” — Report from the 2025 Global Wellness Institute.
Future Outlook: What Happens Next?
As the world moves toward the 2030 deadline for the UN Sustainable Development Goals (SDGs), mental health is gaining unprecedented political and public attention. Global institutions increasingly recognize mental well-being as a foundational pillar of sustainable development and human rights, reinforcing the long-standing principle that there is no health without mental health.
Predicted Milestones (2026–2030)
Right to Disconnect Mandates
Legislation protecting workers’ rest and limiting employer contact outside of working hours is already emerging in several countries, including France, Spain, Italy, and Luxembourg, and is being debated more widely across other regions. Policy momentum suggests broader adoption by the late 2020s, reflecting a growing recognition of rest as a public health necessity rather than a personal luxury.
Mental Health in Primary Care
The World Health Organization and allied agencies are pushing for the integration of mental health services into primary healthcare systems worldwide. Under the SDG 3 framework and the broader universal health coverage agenda, mental health is increasingly being positioned as a core component of routine healthcare, with many countries moving toward earlier screening, community-based care, and reduced reliance on institutional treatment.
The Decline of “Engagement” Metrics
Legal and regulatory scrutiny of social media platforms over mental health harms is intensifying. Governments, public health bodies, and civil society groups are increasingly questioning business models built around addictive engagement. While the scale and legal outcomes of this pressure remain uncertain, digital harms such as excessive screen time, algorithm-driven anxiety, and harmful content exposure are now firmly part of global public health debates.
Neurodivergent-Inclusive Workplaces
A notable shift is underway in how workplaces understand productivity and inclusion. Neurodiversity is increasingly being incorporated into corporate diversity, equity, and inclusion frameworks, reflecting a growing acceptance that different cognitive styles require different environments to thrive. This marks a gradual move away from one-size-fits-all models of work toward more adaptive and humane organizational design.
Rebuilding Society: Why the Mental Health Crisis Demands Systemic Change
The resolution of the “Silent Emergency” will not come from a single breakthrough drug or a more sophisticated algorithm, but from a fundamental reassessment of societal values. As this analysis demonstrates, the mental health crisis of 2026 is the by-product of a world that has prioritized technological acceleration and economic output over the psychological and emotional needs of its people. While the data reveal rising costs and deep systemic gaps, they also point to a moment of transition. Societies are beginning to move away from silence and toward greater transparency and collective accountability.
The future of global stability now depends on shifting from reactive treatment to proactive prevention. This requires a multi-pronged approach: governments must treat mental health as essential social infrastructure; the technology sector must embrace human-centered design that minimizes psychological harm; and workplaces must dismantle the “burnout ceiling” by valuing sustainable engagement over raw working hours. As artificial intelligence becomes more embedded in therapeutic and support systems, preserving genuine human connection must remain the gold standard of care.
Ultimately, the mental health crisis is a call to rebuild the social fabric that has steadily worn thin over the past two decades. Whether through social prescribing, stronger worker protections, or the destigmatization of neurodiversity, the path forward is increasingly clear. If 2026 was the year the emergency was finally heard, then 2027 and beyond must be the years of systemic restructuring. The cost of inaction is too high to measure in economic terms alone; it is measured in the very quality of human life.