Advanced Cardiac Life Support [ACLS] treats people with serious heart emergencies like cardiac arrest, stroke, and life-threatening arrhythmias. Obtaining your ACLS certification is essential for medical professionals, as these skills help save thousands of lives each year. Research shows that about 40%-70% of patients who receive timely ACLS interventions in a hospital setting achieve a return of spontaneous circulation [ROSC].
Preparing for an ACLS exam requires a strong understanding of emergency procedures, medication use, and resuscitation techniques. This blog covers some of the most common questions found in ACLS practice tests with answers to help you succeed.
Most Common Questions in ACLS Practice Tests
ACLS is a set of clinical guidelines used to manage severe cardiac emergencies. If you are preparing for an ACLS exam, you need to understand the content. These are some of the most commonly asked questions in ACLS practice tests with answers.
1. What is the recommended compression-to-ventilation ratio for CPR in adults?
The recommended compression-to-ventilation ratio for adult CPR is 30:2 when there is a single rescuer. This means delivering 30 chest compressions followed by 2 rescue breaths. If an advanced airway is in place [such as an endotracheal tube], continuous compressions should be given at a rate of 100-120 per minute, while rescue breaths are provided every 6 seconds. Proper depth [at least 2 inches] and full recoil of the chest are crucial for effective compressions.
2. What is the first drug given in a cardiac arrest situation?
Epinephrine is the first drug administered during cardiac arrest. It is given at a dose of 1 mg every 3-5 minutes via intravenous [IV] or intraosseous [IO] access. Epinephrine is a potent vasopressor that increases blood flow to vital organs by constricting blood vessels. It also helps improve the chance of restoring spontaneous circulation [ROSC]. If a shockable rhythm is present, defibrillation should be prioritized before administering epinephrine.
3. How do you treat bradycardia in ACLS?
Bradycardia [slow heart rate, usually <50 bpm] is treated based on symptoms. If the patient is unstable [low blood pressure, altered mental status, chest pain], atropine is given at 0.5 mg IV every 3-5 minutes [max dose: 3 mg]. If atropine is ineffective, transcutaneous pacing, dopamine [2-10 mcg/kg/min], or epinephrine infusion [2-10 mcg/min] should be used. The goal is to maintain an adequate heart rate and perfusion.
4. What is the proper sequence of steps in the ACLS systematic approach?
The ACLS systematic approach follows the BLS Survey and Primary and Secondary Assessments. The BLS Survey includes checking responsiveness, activating EMS, checking breathing and pulse, and performing CPR if needed. The Primary Assessment [ABCDE] focuses on the Airway, Breathing, Circulation, Disability [neurological status], and Exposure. The Secondary Assessment involves finding reversible causes using the H’s and T’s [Hypoxia, Hypovolemia, Hydrogen ion [acidosis], Hyper/Hypokalemia, Hypothermia, Tension pneumothorax, Tamponade, Toxins, and Thrombosis].
5. What are the shockable and non-shockable rhythms in ACLS?
Shockable rhythms include ventricular fibrillation [VF] and pulseless ventricular tachycardia [pVT]. These require immediate defibrillation and CPR. Non-shockable rhythms include asystole and pulseless electrical activity [PEA]. For non-shockable rhythms, defibrillation is not effective. Instead, the focus is on high-quality CPR, epinephrine administration, and identifying reversible causes.
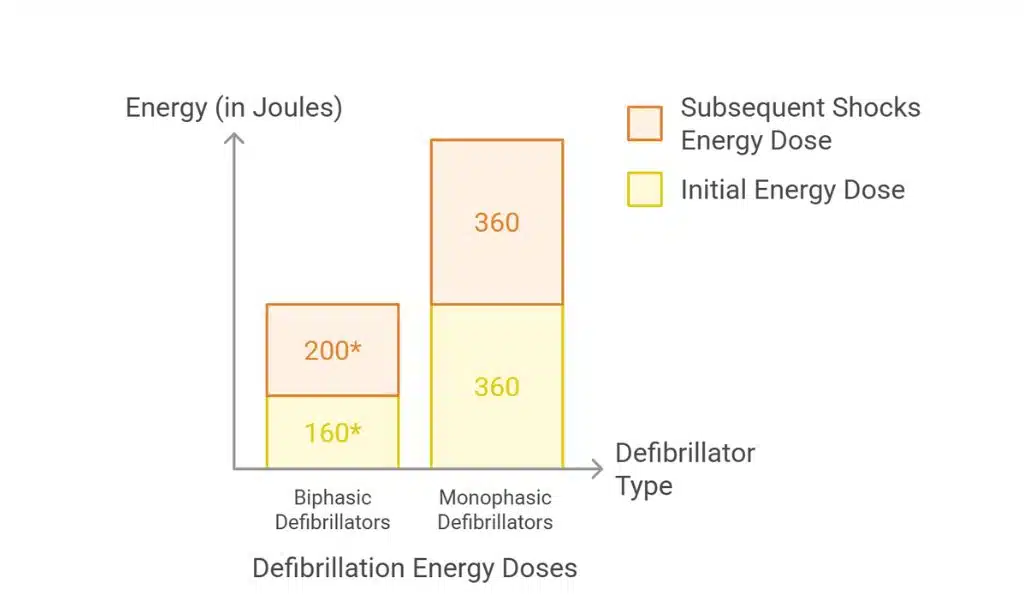
6. What is the correct joule setting for defibrillation in ACLS?
For biphasic defibrillators, the recommended initial energy dose is 120-200 joules [J], depending on the device manufacturer. If the rhythm persists, subsequent shocks should use the same or higher energy level. For monophasic defibrillators, a fixed dose of 360 J is used for all shocks. The goal of defibrillation is to reset the heart’s electrical activity, allowing a normal rhythm to return.
7. What is the recommended post-cardiac arrest care?
Post-cardiac arrest care focuses on stabilizing the patient and preventing further complications. Key steps include maintaining oxygen saturation above 94%, ensuring adequate blood pressure [MAP ≥ 65 mmHg], and using targeted temperature management [32-36°C] to prevent brain damage. Continuous ECG monitoring, managing H’s and T’s, and evaluating for coronary intervention are also essential for improving survival and neurological outcomes.
8. When should you use synchronized cardioversion?
Synchronized cardioversion is used for unstable tachycardia [rapid heart rate causing low blood pressure, chest pain, or altered mental status]. It delivers a timed electrical shock to reset the heart rhythm. Common indications include atrial fibrillation, atrial flutter, supraventricular tachycardia [SVT], and unstable ventricular tachycardia. The energy dose depends on the rhythm: 50-100 J for atrial fibrillation, 50-200 J for atrial flutter and SVT, and 100-200 J for ventricular tachycardia.
9. What is the role of adenosine in ACLS?
Adenosine is used to treat supraventricular tachycardia [SVT], a rapid heart rhythm originating above the ventricles. It works by temporarily blocking electrical conduction through the AV node, helping to restore a normal rhythm. The initial dose is 6 mg IV push, followed by a 12 mg dose if needed. Adenosine must be administered rapidly and followed by a saline flush. It is not effective for atrial fibrillation or ventricular tachycardia.
10. When should you stop resuscitation efforts in ACLS?
Resuscitation efforts should be stopped if there is no return of spontaneous circulation [ROSC] after prolonged CPR, no shockable rhythm, and all reversible causes have been addressed. Additional factors include the patient’s wishes [DNR order], signs of irreversible death, and input from the healthcare team. If ROSC is unlikely despite maximal efforts, stopping CPR is a reasonable decision to prevent unnecessary harm.
11. How do you manage opioid overdose-related respiratory arrest in ACLS?
For opioid overdose, the priority is restoring breathing. Naloxone [0.4-2 mg IV every 2-3 minutes] reverses opioid effects. If respiratory arrest occurs, bag-mask ventilation [10-12 breaths per minute] is necessary. If cardiac arrest follows, high-quality CPR and standard ACLS protocols should be applied. Patients with opioid toxicity require close monitoring, as naloxone’s effects may wear off before the opioid fully clears from their system.
Master ACLS Through Practice and Knowledge!
ACLS is an important skill for healthcare professionals dealing with life-threatening heart emergencies. This blog covered some of the most common questions of ACLS practice tests with answers, including CPR techniques, drug administration, defibrillation, and post-cardiac arrest care. You will be more confident while taking your ACLS exam if you understand these topics. More importantly, this knowledge will prepare you to act quickly and correctly in real-life emergencies.
Regular training and staying updated with ACLS guidelines will ensure that you are always ready to provide the best care possible. Keep reviewing these concepts, and you’ll be well-prepared to handle critical situations effectively.