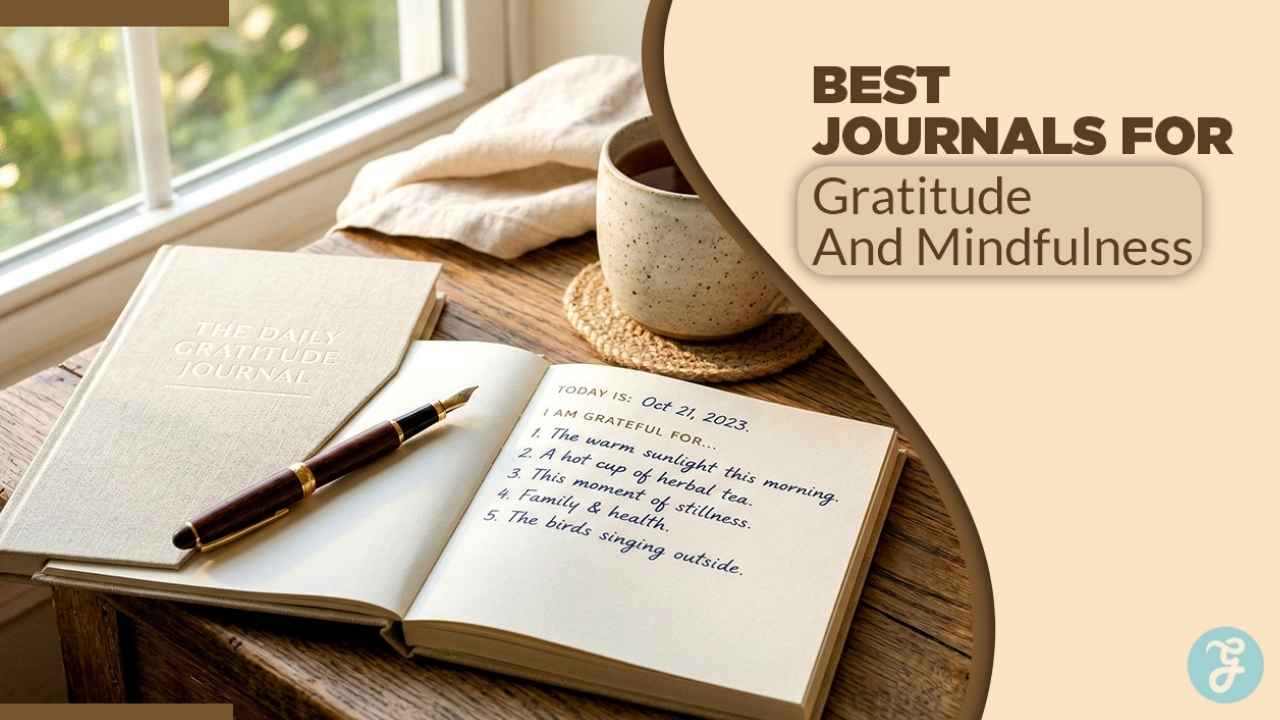
Heart specialists at Intermountain Health in Salt Lake City have uncovered a promising breakthrough in preventing repeat heart attacks through a personalized vitamin D3 supplementation approach. This method, which involves regularly monitoring patients’ blood levels and fine-tuning doses to achieve an optimal range, reduced the risk of a second heart attack by 50% among survivors of an initial event. Unlike previous efforts that relied on fixed doses for everyone, this “target-to-treat” strategy ensures each person’s vitamin D reaches a healthy threshold, addressing individual variations in absorption and needs.
The findings come from a rigorous randomized clinical trial and were presented on November 9 at the 2025 American Heart Association Scientific Sessions in New Orleans, drawing attention from cardiologists worldwide. The study highlights how simple blood tests and dose adjustments can make a big difference without introducing new risks. For heart attack survivors, who face heightened dangers from factors like plaque buildup and inflammation, this could mean a practical way to bolster recovery and long-term heart protection.
Heidi May, PhD, a cardiovascular epidemiologist at Intermountain Health and the principal investigator, expressed optimism about the outcomes during the presentation. We observed no adverse outcomes when giving patients higher doses of vitamin D3 supplementation, and it significantly reduced the risk of another heart attack—these are exciting results,” she said. Dr. May emphasized that while the team is encouraged, validation through larger studies remains essential to build confidence in the approach. Her comments reflect a cautious yet hopeful tone, underscoring the trial’s role as a stepping stone in vitamin D research for cardiovascular care.
This research holds wide-reaching implications, especially since an estimated 50% to 66% of the global population grapples with insufficient vitamin D levels. Low vitamin D has been associated with increased inflammation, weakened immune responses, and poorer vascular health, all of which can exacerbate heart conditions. By focusing on heart attack patients—a group already at elevated risk—the study bridges a gap in how nutritional interventions might fit into standard post-event care protocols. Experts from organizations like the American Heart Association note that such personalized strategies could influence future guidelines for managing chronic heart disease.
Why Vitamin D Deficiency Is on the Rise and Matters for Heart Health?
Vitamin D, often called the “sunshine vitamin,” plays a crucial role in maintaining bone strength, supporting immune function, and regulating cell growth, but its importance for heart health is gaining clearer evidence. Historically, humans obtained sufficient vitamin D through regular exposure to sunlight, where UVB rays trigger the skin to produce it naturally. This process was straightforward for people who spent time outdoors, whether farming, walking, or simply enjoying daily activities under the sun.
However, modern lifestyles have disrupted this natural balance. Urbanization, office-based work, and increased screen time keep many indoors for most of the day, limiting sun exposure to just 10-15 minutes a few times a week—what experts say is often enough for fair-skinned individuals but insufficient for those with darker skin tones or in northern latitudes. Additionally, public health campaigns urging sunscreen use and protective clothing to combat skin cancer have unintentionally contributed to widespread deficiency. The World Health Organization reports that factors like aging, obesity, and certain medications further impair vitamin D production or absorption, affecting billions globally.
In the context of heart health, observational studies spanning decades have consistently linked low vitamin D levels—typically below 20 ng/mL—to higher rates of hypertension, diabetes, and coronary artery disease. For instance, research from the Framingham Heart Study showed that individuals with severe deficiency faced up to a 60% greater risk of cardiovascular events. Vitamin D helps by reducing arterial stiffness, curbing inflammation markers like C-reactive protein, and supporting endothelial function—the lining of blood vessels that prevents plaque formation.
Despite these associations, earlier clinical trials disappointed by failing to demonstrate benefits. Most provided standard doses of 400-2,000 IU daily without verifying if blood levels actually rose, often because some people metabolize vitamin D inefficiently due to genetics or gut health issues. Intermountain researchers hypothesized that the missing piece was personalization: aiming for a specific serum level rather than assuming equal response across participants. This insight stems from broader endocrine research, including guidelines from the Endocrine Society, which advocate for 30-50 ng/mL as optimal for overall health, particularly in at-risk groups like heart patients.
Dr. May elaborated on this shift: “Previous studies just gave patients supplementation without regularly checking blood levels of vitamin D to determine what supplementation achieved. With more targeted treatment, when we checked exactly how supplementation was working and made adjustments, we found that patients had their risk of another heart attack cut in half.” Her explanation aligns with emerging consensus that vitamin D’s protective effects on the heart—such as lowering parathyroid hormone, which can strain the cardiovascular system—only activate when levels are consistently maintained in the ideal range.
How the TARGET-D Study Was Designed and Conducted?
The Intermountain study, known as the TARGET-D trial, was a prospective, randomized controlled trial that spanned from April 2017 to May 2023, enrolling 630 patients across multiple facilities in Utah. Participants were adults who had experienced a myocardial infarction—a heart attack—within one month of joining, making it highly relevant to real-world post-event care. The average age was 63 years, with about 80% being male, reflecting typical demographics for heart attack survivors, though researchers noted the need for more diverse inclusion in future work.
At baseline, a striking 85-87% of enrollees had insufficient vitamin D3 levels below 40 ng/mL, with an average of around 27 ng/mL—well under what many experts consider protective. This prevalence underscores the trial’s timeliness, as routine screening for vitamin D isn’t yet standard in cardiology, despite calls from bodies like the National Institutes of Health. Patients were randomly assigned to one of two arms: a control group receiving usual care without vitamin D intervention, and an active treatment group focused on targeted supplementation.
For the treatment group, the protocol was meticulous. The primary goal was to elevate 25-hydroxyvitamin D (the main circulating form) to above 40 ng/mL, a threshold chosen based on prior evidence linking it to reduced cardiovascular inflammation and improved outcomes. Initial dosing started high for most: over 50-60% needed 5,000 IU daily of vitamin D3 (cholecalciferol, the preferred form for supplementation), compared to general recommendations of 600-800 IU from the U.S. Institute of Medicine for healthy adults. This higher start was necessary because deficiency often requires a “loading dose” to replenish stores quickly, followed by maintenance.
Monitoring was key to safety and efficacy. Blood tests occurred annually for those at target levels, but every three months for anyone dipping below, allowing real-time dose adjustments—up to 10,000 IU if needed, though most stabilized at lower amounts. No participants reported hypercalcemia or other toxicities, even at elevated intakes, which is reassuring given vitamin D’s fat-soluble nature that can lead to buildup if unchecked. The trial adhered to ethical standards, with institutional review board approval and informed consent, ensuring participants understood the focus on vitamin D alongside their standard medications like statins or blood thinners.
Follow-up extended to March 2025, tracking events via electronic health records and clinic visits. This long horizon—up to eight years for some—provided robust data on recurrence, with statistical analysis using intention-to-treat principles to account for dropouts (about 10%, mostly unrelated to the intervention).
Key Findings, Limitations, and Implications for Patients
Among the 630 participants, 107 experienced a major adverse cardiovascular event (MACE), defined as recurrent heart attack, stroke, hospitalization for heart failure, or cardiovascular death. Overall MACE rates showed no statistically significant difference between groups—around 17% in both—suggesting targeted vitamin D doesn’t broadly shield against all heart threats. However, the standout result was in recurrent myocardial infarctions: the treatment group had a 3.8% rate compared to 7.9% in controls, a 52% relative reduction that held up in subgroup analyses, including by age and baseline severity.
This specificity to heart attacks is intriguing. Researchers attribute it to vitamin D’s targeted anti-inflammatory effects on coronary arteries, potentially stabilizing plaques that cause blockages. No differences emerged in strokes or heart failure, possibly due to the sample size or the trial’s focus on recent heart attack patients rather than broader heart disease. Adverse events were minimal, with only minor gastrointestinal upset in a few, reinforcing vitamin D3’s safety profile when monitored.
Limitations include the single-center design, predominantly white male cohort, and preliminary status—results are from an abstract, not a full peer-reviewed paper. External factors like diet, exercise, or concurrent therapies could influence outcomes, though randomization helped balance these. Still, the findings challenge past null results from trials like VITAL or ViDA, which used uniform dosing and didn’t prioritize high-risk groups.
For patients, the message is empowering: if you’ve had a heart attack, discuss vitamin D testing with your doctor. A simple blood draw can reveal deficiency, and tailored supplementation—starting at 2,000-5,000 IU under guidance—might offer accessible protection. Cardiologists like Cheng-Han Chen, MD, from MemorialCare, praise the personalization, noting it could integrate into routine follow-up without high costs.
Next Steps in Vitamin D and Heart Research
Building on TARGET-D, Intermountain plans a multicenter phase III trial with thousands of participants to confirm the 50% risk reduction and probe effects on strokes, heart failure, and overall mortality. This expansion will include diverse ethnicities, women, and longer follow-up to address current gaps. Funding from the National Heart, Lung, and Blood Institute could accelerate it, potentially leading to guideline updates by 2027-2028.
In the interim, experts recommend against self-dosing high amounts; instead, aim for food sources like salmon (provides 400-600 IU per serving) or fortified milk, combined with safe sun exposure. The American Heart Association supports awareness of vitamin D in heart health education, viewing this as part of a holistic strategy including diet, exercise, and meds. As Dr. May concluded, “A larger study group will allow us to more fully evaluate whether targeted vitamin D management can reduce not only repeat heart attacks but also other forms of cardiovascular disease.” These efforts could transform how we prevent heart events, making vitamin D a cornerstone of personalized cardiology.