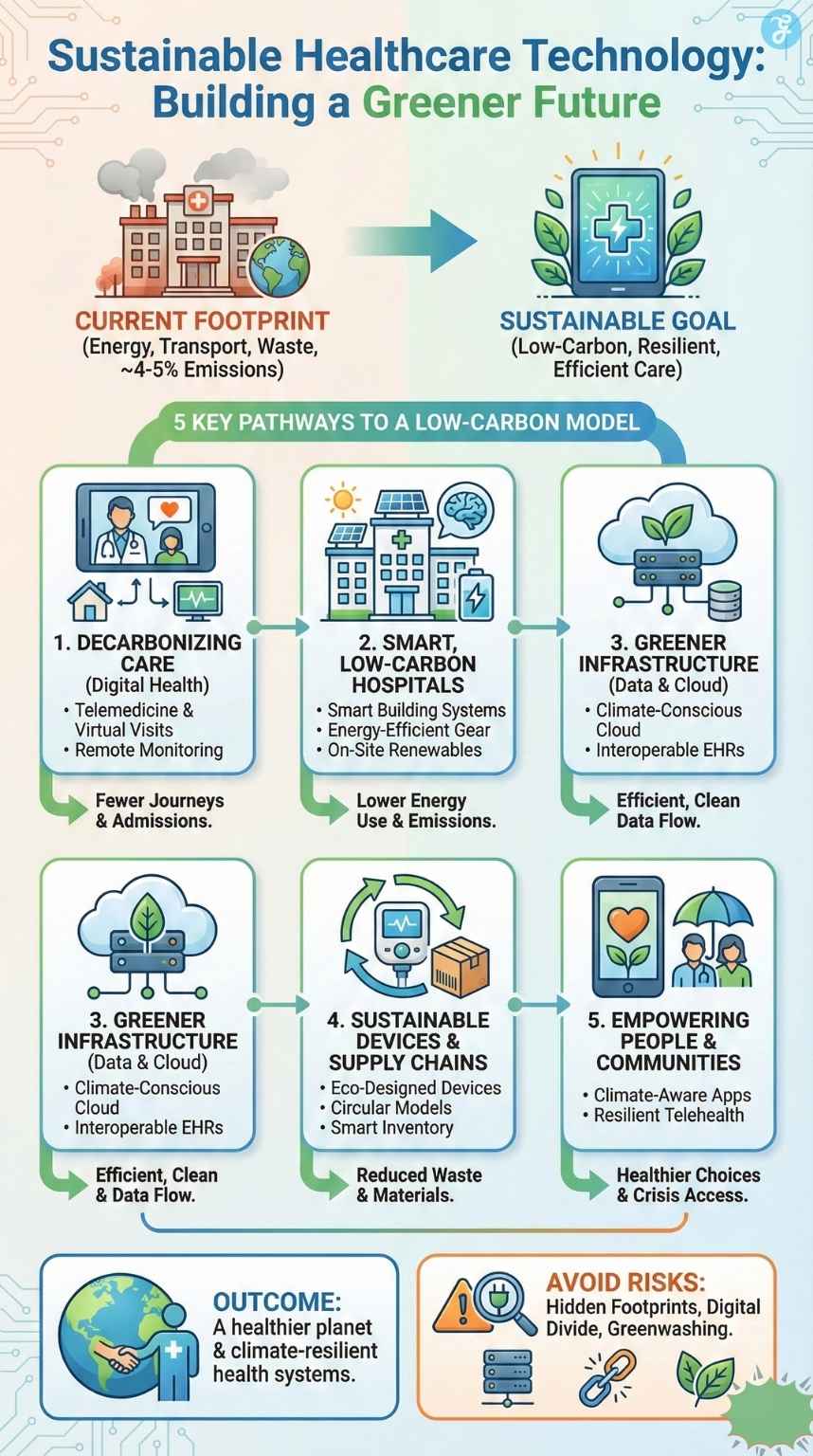
Healthcare keeps people alive and well, but it also comes with a hidden environmental cost. Globally, the health sector is responsible for roughly 4–5% of total greenhouse gas emissions, making it comparable to the aviation industry in climate impact.
As populations grow and health systems become more digital, the question is simple: can we protect people’s health without harming the planet? This is where sustainable healthcare technology comes in. It uses digital tools, smarter devices, and cleaner infrastructure to improve care while cutting emissions, waste, and resource use.
Let’s explore 20 practical ways sustainable healthcare technology is already helping to build a greener future. You will see how telemedicine, smart hospitals, cleaner data centers, circular devices, and empowered patients can together move healthcare toward a low-carbon, climate-resilient model.
What Is Sustainable Healthcare Technology and Why It Matters
Sustainable healthcare technology is the use of digital health tools, medical devices, and data systems that improve patient outcomes while reducing environmental harm across their whole life cycle. That means considering energy use, materials, transport, and waste from design to disposal.
The healthcare sector’s climate footprint comes from many sources: energy-hungry buildings, medical products and devices, pharmaceuticals, transport, and waste. A global analysis showed that if healthcare were a country, it would be the fifth-largest emitter in the world.
At the same time, climate change is already a health crisis. Heatwaves, air pollution, floods, and new disease patterns are increasing hospital admissions and straining systems that are often not designed to cope with extreme events.
Sustainable healthcare technology sits at the intersection of these challenges.
It aims to:
- Reduce emissions and pollution from care delivery
- Build climate-resilient services that work during shocks
- Use resources more efficiently, easing financial pressure
- Improve equity so digital innovations do not leave people behind
Why Sustainable Healthcare Technology Matters
| Aspect | Key Point |
| Climate footprint | The health sector emits ~4–5% of global greenhouse gases |
| Main emission sources | Energy, buildings, supply chains, transport, and waste |
| Health impacts of climate | More heat-related illnesses, pollution, and extreme weather events |
| Role of technology | Cut emissions, improve resilience, and support more efficient care |
| Equity consideration | Must ensure digital tools are accessible and inclusive |
Decarbonizing Care Delivery with Digital Health
Digital health is often the first thing people think of when they hear sustainable healthcare technology. Done well, it can dramatically cut travel, reduce unnecessary appointments, and shift care from hospitals to homes.
1. Telemedicine and Virtual Visits
Telemedicine allows patients to connect with clinicians via video or phone instead of traveling to a clinic. Large studies in the United States found that millions of virtual visits can save several million kilograms of CO₂ emissions every month by avoiding car journeys.
Another analysis of telemedicine visits in oncology showed significant reductions in emissions per appointment when virtual care replaced in-person visits, especially for patients living far from hospitals.
Telehealth is not a full replacement for physical care. Some conditions still need in-person exams, imaging, or procedures. But if health systems reserve in-person visits for when they are truly needed, telemedicine becomes one of the clearest climate wins in modern care.
2. Remote Monitoring and Hospital-at-Home
Remote patient monitoring uses connected devices to track vital signs such as blood pressure, oxygen saturation, or glucose levels from home. This can prevent avoidable hospital admissions and allow early intervention when readings worsen.
Hospital-at-home programs go further, providing hospital-level care at home with remote monitoring, nurse visits, and virtual rounds by doctors. Fewer overnight stays can reduce building energy demand and the resources used per patient episode, while often improving comfort and satisfaction.
3. Smart Digital Triage
AI-supported chatbots, symptom checkers, and online triage tools help patients decide if they need urgent care, routine appointments, or self-care. When carefully designed and supervised, they can reduce unnecessary emergency visits and diagnostic overuse, which lowers emissions and costs.
4. Preventive Digital Health Tools
Wearables and mobile health apps encourage physical activity, better sleep, healthy diets, and treatment adherence. Prevention and early intervention mean fewer severe complications and fewer resource-intensive hospital stays later in life.
5. Virtual Rehabilitation and Mental Health Services
Virtual physiotherapy sessions, online rehabilitation programs, and tele-mental-health services remove the need for frequent travel to specialist centers. Evidence shows these models can match traditional care for many conditions, with added convenience for patients.
Digital Health for Lower-Carbon Care
| Sub-area | Main Benefit |
| Telemedicine | Cuts travel-related emissions and time |
| Remote monitoring | Prevents admissions and allows hospital-at-home care |
| Smart digital triage | Reduces unnecessary emergency and clinic visits |
| Preventive digital health | Avoids late-stage, resource-intensive treatments |
| Virtual rehab and e-mental health | Less travel and more flexible, continuous care |
Smart, Low-Carbon Hospitals and Clinics
Hospitals are among the most energy-intensive buildings in any city. They operate 24/7, require strict climate control, and house complex equipment. Smart building technologies can make them far more efficient.
6. Smart Building Management Systems
Intelligent building management systems act like the nervous system of a hospital: they monitor heating, cooling, ventilation, lighting, and safety systems in real time. Smart metering and analytics show where energy is wasted, and help engineers optimize settings without compromising safety or comfort.
In the United States, hospitals account for around 9% of commercial building energy use, so even small efficiency gains translate into large savings and climate benefits.
7. Energy-Efficient Medical Equipment
Newer imaging systems, sterilizers, and support equipment are more energy-efficient and often have “eco modes” that reduce consumption when idle. When hospitals consider lifetime energy usage and not just purchase price, low-energy equipment becomes a smart choice.
8. On-Site Renewable Energy and Smart Cooling
Many hospitals are installing solar panels, efficient heat pumps, and low-carbon energy centers. Some now use thermal energy storage or “ice batteries” that freeze water at night when grid demand is lower and then use the stored cold to cool buildings during the day. This reduces peak electricity use and emissions while maintaining stable temperatures in operating rooms and wards.
9. Smart Water, Waste, and Food Management
Digital sensors can track water leaks, monitor consumption, and support conservation. Waste management software helps hospitals improve segregation between infectious, recyclable, and general waste, which reduces incineration and landfill. Food service platforms can cut food waste by matching production to actual demand.
10. Digital Twins for Planning and Operations
A digital twin is a virtual model of a hospital that simulates patient flows, staff movements, and energy use. Planners can test different layouts, schedules, and retrofits on the twin before making expensive changes in real life. This avoids costly design errors and helps hospitals invest in the most climate-friendly options.
Smart Hospitals and Climate Benefits
| Area | Example Action | Impact |
| Smart building management | Real-time control of HVAC and lighting | Lower energy use and emissions |
| Efficient medical devices | Low-energy imaging and sterilization equipment | Reduced electricity consumption |
| On-site renewables | Solar, heat pumps, ice-battery cooling | Cleaner, more resilient power |
| Water and waste management | Sensors and digital waste tracking | Less waste and better recycling |
| Digital twins | Simulated layouts and workflows | Smarter, lower-carbon investments |
Greener Data, Cloud, and Digital Infrastructure
Every virtual visit, scan, and lab result generates data. Behind the scenes, servers, networks, and devices consume energy.
11. Climate-Conscious Cloud Strategies
Moving hospital data centers to cloud providers that run on renewable energy and use advanced cooling can significantly cut emissions. Many large cloud companies now report the share of their data centers powered by clean energy and offer tools to track carbon footprints.
For sustainable healthcare technology to be truly green, procurement teams should consider not only functionality and price, but also the provider’s climate strategy.
12. Interoperable Electronic Health Records
Interoperable electronic health records (EHRs) allow health professionals to access the same information across different facilities. This reduces duplicate tests and imaging, cuts paperwork, and improves care coordination. Fewer unnecessary scans and lab tests mean less energy, materials, and waste.
13. Sustainable AI in Healthcare
AI can help with diagnosis, triage, imaging analysis, and logistics. But training and running large models can be energy-intensive. Climate-aware AI means choosing efficient algorithms, focusing on high-value use cases, and using green data centers.
Greener Digital Infrastructure
| Component | Sustainability Strategy |
| Cloud services | Choose providers with a high renewable share |
| Data centers | Efficient cooling and hardware management |
| EHR systems | Interoperability to avoid duplicate tests |
| AI tools | Efficient models and targeted use cases |
Sustainable Devices, Diagnostics, and Supply Chains
A large share of healthcare’s carbon footprint comes from the production, transport, and disposal of medical products and devices.
14. Eco-Designed Medical Devices and Packaging
Manufacturers are beginning to design devices with fewer materials, more recyclable components, and minimal packaging. Reusable surgical instruments, lower-impact plastics, and smart packaging that reduces waste all contribute to cleaner supply chains.
15. Circular Models and Take-Back Schemes
Instead of buying equipment outright, some hospitals now lease devices under “product-as-a-service” models. Suppliers retain ownership, refurbish equipment, and recover valuable materials at the end of life. This encourages longer product lifetimes and careful maintenance.
16. Smart Inventory Management
Using barcodes, RFID tags, and predictive analytics, hospitals can better match stock levels to actual usage. This reduces expired medicines, unused implants, and over-ordering of single-use items, which lowers waste and associated emissions.
17. Low-Carbon Diagnostics and Point-of-Care Testing
Point-of-care diagnostic devices bring testing closer to patients, reducing the need for sample transport and centralized lab processing for certain conditions. Combined with efficient lab workflows, this can reduce energy use while maintaining accuracy and speed.
Greener Devices and Supply Chains
| Focus Area | Example Change | Benefit |
| Device design | Reusable or modular devices | Less material and e-waste |
| Packaging | Reduced and recyclable materials | Lower plastic and cardboard use |
| Business model | Leasing and take-back schemes | Longer lifetimes, more reuse |
| Inventory | Data-driven stock management | Fewer expired or unused items |
| Diagnostics | Point-of-care and optimized lab processes | Less transport and energy use |
Empowering Patients and Communities with Green Health Tech
Sustainable healthcare technology is not only about hospitals and IT departments. It also supports patients and communities in making healthier, climate-friendly choices.
18. Health Apps with Climate-Aware Features
Some health apps now combine behavior change (like walking instead of driving, eating more plant-rich diets, or quitting smoking) with insights on carbon savings. They show how personal health actions can also reduce emissions, linking wellbeing and climate action in a clear, motivating way.
19. Climate-Resilient Telehealth for Vulnerable Groups
When extreme heat, flooding, or air pollution make travel unsafe, telehealth can keep care accessible. Digital tools help maintain continuity of treatment, protect people from exposure, and relieve pressure on overloaded emergency departments.
20. Community Data Platforms
Digital platforms that combine health data with environmental information (such as air quality, temperature, or pollen levels) can guide local public health actions. Authorities can target interventions, early warnings, and outreach to communities at the highest risk.
Patient and Community-Level Benefits
| Tool or Approach | How It Helps People and Planet |
| Health and climate apps | Connect health behaviors with carbon savings |
| Telehealth in crises | Maintain care during heatwaves or floods |
| Community data platforms | Targeted, evidence-based public health actions |
Risks, Trade-Offs, and Avoiding Greenwashing
Sustainable healthcare technology brings clear benefits, but there are important risks and trade-offs.
Hidden Footprints
The devices, servers, and networks behind digital health have their own environmental footprints. Manufacturing electronics uses metals, plastics, and energy; data centers consume power and water for cooling. Without careful design and procurement, digital health could simply shift emissions from roads and buildings to factories and servers.
Equity and the Digital Divide
Not everyone has reliable internet access, digital skills, or suitable devices. If telemedicine and digital tools become the default without alternatives, they can widen health inequalities instead of closing them. Climate-conscious solutions must also be equity-conscious.
Avoiding Greenwashing
Some products are marketed as “green” without strong evidence. To avoid greenwashing, health systems can:
- Ask for lifecycle assessments and carbon data
- Request independent evaluations, not just vendor claims
- Include environmental criteria in health technology assessments, alongside safety and effectiveness
Key Risks and How to Respond
| Risk | Example Issue | Response Strategy |
| Hidden footprint | Energy-intensive data centers | Choose green providers and efficient designs |
| Digital divide | Poor access in rural areas | Offer hybrid options and digital support |
| Greenwashing | Unproven “eco” claims | Demand transparent, evidence-based metrics |
How to Accelerate Sustainable Healthcare Technology
To unlock the full potential of sustainable healthcare technology, action is needed from policymakers, providers, and tech companies.
Aligning Health and Climate Policy
Many countries and health systems now have net-zero or decarbonization targets. Linking these goals to digital health strategies ensures that every new app, system, or device is assessed for environmental as well as clinical impact.
Standards, Metrics, and Reporting
It is hard to manage what is not measured. Health systems can start by tracking:
- Emissions per patient visit or procedure
- Energy use per square meter in buildings
- Device lifetimes and e-waste volumes
These metrics help leaders decide where sustainable healthcare technology investments will have the biggest effect.
Skills and Culture
Health professionals need digital and climate literacy to make good use of these tools. New training initiatives in Europe, for example, focus on building digital health data skills and promoting sustainable healthcare practices among future clinicians.
A culture shift is also needed: sustainability should be seen as part of quality and patient safety, not an optional extra.
Levers for Faster Adoption
| Lever | Example Action |
| Policy | Include climate criteria in digital health plans |
| Metrics | Track emissions and energy per care activity |
| Procurement | Choose suppliers with clear net-zero roadmaps |
| Training | Build digital and climate skills into curricula |
| Culture | Treat sustainability as core to quality and safety |
FAQs About Sustainable Healthcare Technology
What is sustainable healthcare technology?
Sustainable healthcare technology is any digital tool, device, or data system that improves health outcomes while reducing environmental harm over its full life cycle. It covers everything from telemedicine platforms and EHR systems to smart building controls and eco-designed medical devices.
Is digital health always better for the environment?
Not always. Telemedicine and remote monitoring can cut travel emissions and reduce pressure on buildings, but they still rely on energy-using devices and data centers. The net benefit depends on factors such as distance avoided, type of device, and the electricity mix. Well-designed sustainable healthcare technology maximizes the gains while minimizing the digital footprint.
How can hospitals start with sustainable healthcare technology?
Hospitals can begin by auditing where emissions are highest, often in energy use and supply chains. Then they can introduce telehealth where clinically appropriate, optimize building management, choose greener cloud providers, and add environmental criteria to new technology purchases. Starting with a few high-impact projects builds experience and support.
What can patients do to support greener healthcare?
Patients can opt for virtual visits when safe and convenient, use digital records and portals instead of paper, keep appointments to avoid wasted slots, and return devices or e-waste through proper channels. Small choices at the individual level add up when millions of people participate.
Bottom Line: A Healthier Planet Needs Sustainable Healthcare Technology
Healthcare exists to protect human life, but it must do so within planetary limits. Today’s health systems emit a significant share of global greenhouse gases, yet they also hold some of the most powerful tools to reduce that footprint.
Sustainable healthcare technology brings together digital health, smart hospitals, greener devices, and empowered patients into one coherent approach. Used wisely, it can cut emissions, lower costs, and improve resilience to climate shocks while keeping or even improving care quality.
The path forward is clear: design and choose technologies that are evidence-based, low-carbon, and equitable; measure their impact; and make sustainability part of everyday clinical and management decisions. If we succeed, sustainable healthcare technology will help deliver not only healthier lives, but a healthier planet for future generations.