Chinese researchers have accomplished a groundbreaking feat by successfully reversing both type 1 and type 2 diabetes in human patients through innovative stem cell therapy, marking the first time such a complete reversal has been achieved. This pioneering work involves reprogramming a patient’s own cells into functional insulin-producing beta cells, which are then transplanted to restore the body’s natural ability to manage blood sugar levels without the need for lifelong insulin injections or medications. The achievement, emerging from leading institutions like Tianjin First Central Hospital and the Shanghai Institute of Endocrine and Metabolic Diseases, signals a potential revolution in diabetes treatment, offering renewed hope to the more than 500 million people globally affected by the condition.
This development stems from years of dedicated research, building on earlier stem cell experiments but advancing to human applications with remarkable speed, thanks to China’s robust investment in biotechnology and regenerative medicine. Early clinical trials have demonstrated not just symptom relief but genuine cellular-level recovery, where transplanted cells integrate into the body, form their own blood supply, and respond dynamically to glucose fluctuations. As trials expand, this therapy could redefine diabetes from a chronic, incurable illness to one that patients can overcome, potentially easing the massive economic and personal burdens it imposes worldwide.
The Global Burden of Diabetes and Why This Matters
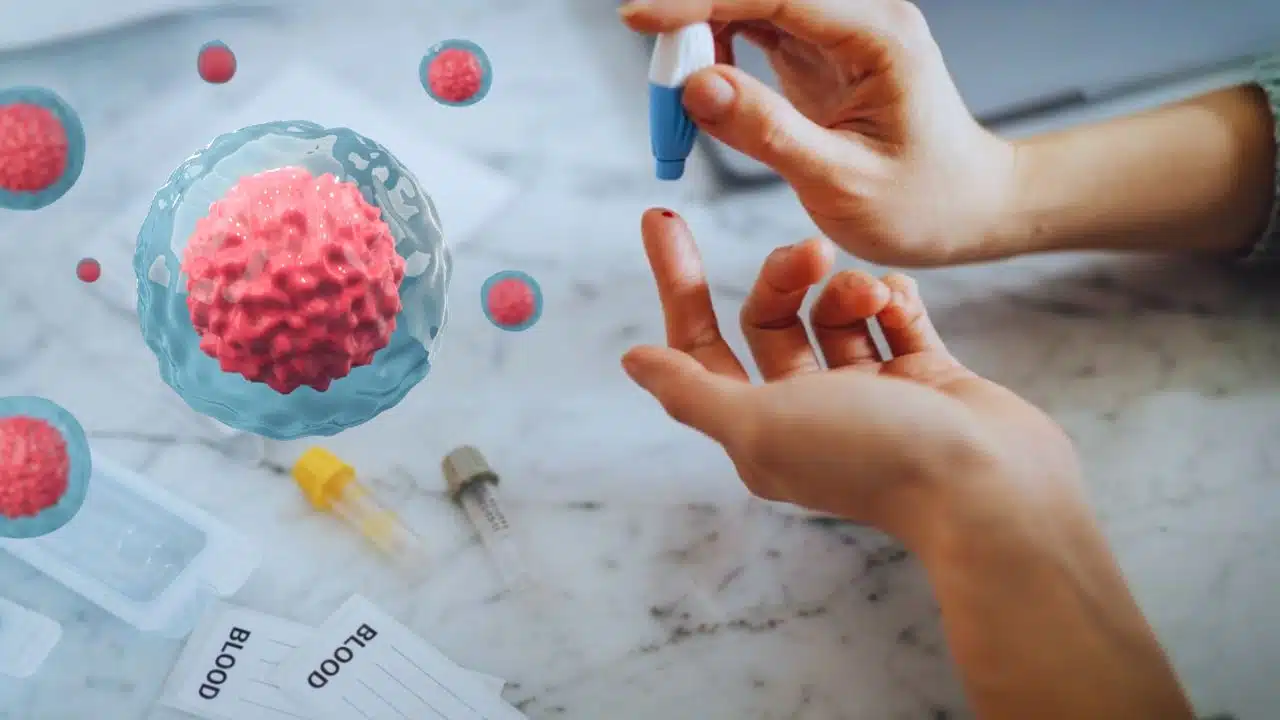
Diabetes remains one of the most pervasive health crises today, affecting over 500 million adults and projected to reach 783 million by 2045, according to the International Diabetes Federation. In type 1 diabetes, an autoimmune disorder typically diagnosed in childhood or young adulthood, the immune system mistakenly destroys the insulin-producing beta cells in the pancreas, forcing patients into immediate and permanent reliance on external insulin to survive. This leads to frequent blood sugar monitoring, multiple daily injections, and a constant risk of life-threatening highs or lows, often resulting in complications like kidney failure, heart disease, neuropathy, and vision impairment if not meticulously managed.
Type 2 diabetes, which accounts for about 90% of cases, arises from a combination of insulin resistance—where cells fail to respond properly to insulin—and the eventual exhaustion of beta cells, often exacerbated by factors such as obesity, sedentary lifestyles, genetics, and aging. While it can sometimes be managed through diet, exercise, and oral medications in its early stages, many patients progress to insulin dependence, facing similar daily struggles and long-term risks as those with type 1. Globally, diabetes contributes to over 1.5 million deaths annually and imposes healthcare costs exceeding $966 billion, with much of that spent on ongoing treatments rather than cures.
For patients, the reality is exhausting: constant dietary restrictions, the fear of hypoglycemia during sleep or exercise, and the emotional toll of a disease that disrupts every aspect of life, from work to family. Traditional therapies, while life-saving, only mask the problem by supplementing insulin or improving sensitivity; they do not regenerate the lost cells or halt the disease’s progression. This Chinese breakthrough addresses that core deficiency, offering a path to insulin independence and reduced complication risks, which could transform quality of life and alleviate the strain on healthcare systems strained by rising cases, particularly in Asia where type 2 prevalence is surging due to urbanization and dietary shifts.
The Science Behind the Stem Cell Therapy
At the heart of this therapy is the use of induced pluripotent stem cells (iPSCs), a Nobel Prize-winning technology discovered in 2006 that allows ordinary adult cells to be reprogrammed into a versatile, embryonic-like state capable of differentiating into any cell type. In these trials, researchers harvest autologous cells—typically from the patient’s fat tissue via liposuction or bone marrow extraction—to minimize rejection risks and eliminate the need for lifelong immunosuppressive drugs that often accompany donor-based transplants.
The process unfolds in specialized labs: the collected cells are treated with specific chemical cocktails or genetic factors to revert them to iPSCs, a step that takes about two weeks. These iPSCs are then guided through a multi-stage differentiation protocol mimicking pancreatic development, involving growth factors like activin A, retinoic acid, and Wnt inhibitors to coax them into functional islet clusters—mini-organs containing beta cells that produce insulin, alpha cells for glucagon, and supporting delta cells. This lab-culturing phase lasts around 40 to 60 days, during which the cells are rigorously tested for purity, potency, and safety to ensure they express key markers like PDX1 and NKX6.1 for beta cell identity.
Once ready, the islet clusters—numbering in the millions—are transplanted via minimally invasive procedures, such as injection into the abdominal anterior rectus sheath or under the skin, where they engraft, vascularize, and connect to the body’s blood supply. In a unique Chinese innovation, some protocols integrate Traditional Chinese Medicine (TCM) elements, like herbal extracts to enhance cell viability and reduce inflammation, alongside Western biotech standards, creating a holistic approach that supports faster integration. The transplanted cells then sense rising blood glucose through glucose transporters like GLUT2 and respond by secreting insulin in precise pulses, restoring the body’s natural feedback loop via mechanisms such as the KATP channel for glucose-stimulated secretion.
This patient-specific method contrasts with earlier allogeneic transplants from cadavers, which faced donor shortages and immune challenges; here, the therapy leverages the patient’s own biology for a more sustainable, personalized solution. Ongoing refinements include CRISPR gene-editing to make beta cells more resistant to autoimmune attacks in type 1 cases or to boost insulin sensitivity in type 2, potentially making the therapy even more effective for diverse patient profiles.
Impressive Results from Initial Clinical Trials
The first wave of results from these trials has been nothing short of transformative, providing concrete evidence of the therapy’s potential. In a landmark case at Tianjin First Central Hospital, a 25-year-old woman diagnosed with type 1 diabetes over a decade earlier received the transplant in mid-2024; within just 75 days, her endogenous insulin production resumed, allowing her to discontinue all external insulin. Follow-up monitoring showed her HbA1c dropping from 8.6% to a normal 5.8%, with stable fasting and post-meal glucose levels, and she has remained insulin-independent for more than 18 months as of late 2025, with no signs of rejection or tumor formation.
Expanding to type 2, trials at the Shanghai Institute involved a 59-year-old man with a 25-year history of the disease and insulin dependence; after receiving beta cell clusters derived from his adipose tissue, he achieved insulin freedom in 11 weeks and has sustained it for over a year, alongside improvements in weight, energy levels, and neuropathy symptoms. Broader studies, including one with over 700 participants across multiple centers, report that 60% of type 2 patients achieve partial or full remission within 8-12 months, with average A1C reductions of 1.8-3.2%, and many experiencing enhanced beta cell function confirmed via C-peptide tests measuring natural insulin output.
In type 1 trials involving three initial patients led by Peking University researchers, all participants showed positive outcomes: the second and third reached one-year insulin independence by November 2025, with engrafted cells producing insulin in response to meals and exercise. Side effects have been minimal—mostly mild abdominal discomfort during transplant— and no serious adverse events like infections or malignancies have occurred, thanks to the autologous nature and strict quality controls. These results, published in prestigious journals like Cell, have been hailed by experts such as Dr. Douglas Melton of Harvard as “a game-changer,” highlighting how the therapy restores not just insulin but the full spectrum of islet hormone regulation.
Additional data from registered trials on platforms like ChiCTR reveal sustained glucose control in follow-ups, with patients reporting fewer hypoglycemic episodes and better overall well-being, underscoring the therapy’s role in preventing downstream complications like cardiovascular disease.
Challenges, Future Developments, and Path to Global Availability
While the early successes are encouraging, scaling this therapy faces several hurdles that researchers are actively addressing. The current process requires sophisticated facilities for cell culturing, limiting access to major urban centers in China, and costs range from $12,000-$18,000 for basic stem cell infusions to $25,000-$400,000 for full iPSC-based islet transplants, though these may decrease with automation and mass production techniques. Long-term monitoring is essential to track durability—current data spans up to two years, but five- to ten-year studies are needed to confirm if the cells evade autoimmune recurrence in type 1 or resist the progressive factors in type 2.
Regulatory pathways in China have accelerated approvals through initiatives like the Beijing-Tianjin-Hebei Health Valley, but international bodies such as the FDA and EMA will require Phase III trials with larger, diverse cohorts to validate efficacy across ethnicities and ages. Ethical considerations, including equitable access for low-income regions where diabetes hits hardest, and potential disruptions to the $20 billion insulin market, could influence global adoption, prompting calls for collaborative international trials in Europe, the UAE, and Latin America.
Looking ahead, expansions include combining the therapy with CRISPR for immune-protected cells, pancreatic scaffold implants for better engraftment, and AI-optimized differentiation protocols to shorten production to under a month. Phase IV global trials are underway, with hopes of initial approvals in select countries by 2027-2028, potentially making this a standard option for newly diagnosed patients to prevent years of management. Patients interested should consult endocrinologists at specialized centers, as eligibility often favors those with stable disease and no severe comorbidities.
A New Era in Regenerative Medicine
This Chinese innovation exemplifies the power of regenerative medicine to heal at the source, turning diabetes from an inevitable lifelong challenge into a potentially curable condition. By harnessing the body’s own repair mechanisms, the therapy not only frees patients from daily regimens but also averts the cascade of secondary health issues, fostering fuller lives and healthier societies.
As research progresses, it paves the way for similar advances in other endocrine disorders, proving that true cures lie in restoring function rather than endless intervention. With continued global collaboration, the dream of diabetes eradication draws ever closer, backed by science that prioritizes human potential over perpetual treatment.