Living with type 2 diabetes for more than a decade has often felt like walking a tightrope—juggling blood sugar, injections, side effects, diet, and exercise while still trying to live fully.
Recently, I started a new chapter with tirzepatide. Below is my honest story—what I changed, what worked, what didn’t—and how this weekly injection fits into real life with diabetes.
Along the way, I’ll share evidence and current guidance so you can compare my experience with what large clinical studies show.
What Is Tirzepatide?
Tirzepatide is a relatively new prescription medication designed to help manage type 2 diabetes and support weight loss. It belongs to a unique class of drugs that act as dual receptor agonists—targeting both GLP-1 and GIP receptors.
These are hormones naturally found in the body that regulate blood sugar and appetite. Tirzepatide works by enhancing insulin release when needed and reducing hunger, helping people achieve better control over their blood glucose and body weight.
My Earlier Experience with Semaglutide
I began my journey with semaglutide in early 2023 under the guidance of Dr. Mohammad Sayem, a renowned internal medicine specialist in Bangladesh. At that time, it felt like a big step toward better diabetes management, and with his expertise, I was hopeful about the changes ahead.
In my previous account of living with diabetes, I detailed how semaglutide—under brand names such as Fitaro and Orsema in Bangladesh—proved both a boon and a challenge. While it helped me achieve significant improvements in blood sugar control and triglyceride levels, and enabled consistent weight loss, the medication also aggravated my pre-existing IBS symptoms.
I experienced persistent gastric discomfort, irregular bowel movements, nausea, and even dilution issues that ultimately led me to undergo gallbladder surgery at an unusually young age. This dual-edged nature of Semaglutide underscores the importance of monitoring and adjusting treatment based on individual responses.
Why Tirzepatide Caught My Attention
Tirzepatide is a once-weekly injection that activates two incretin pathways (GLP-1 and GIP), helping the body release insulin when glucose is high, reduce appetite, and slow stomach emptying.
In the U.S. it’s branded as Mounjaro for type 2 diabetes and Zepbound for obesity. Large trials have shown meaningful A1C reductions and significant weight loss—often more than with single-pathway GLP-1 drugs.
Quick evidence snapshot
- A1C: In head-to-head trials vs semaglutide 1 mg, tirzepatide produced greater A1C reductions at all doses.
- Weight: In people with obesity without diabetes, average weight loss reached ~20% at 72 weeks at higher doses.
- Lipids: Meta-analyses show improvements in triglycerides and cholesterol with a dose-response trend.
Guidelines: The 2025 ADA Standards of Care include dual GIP/GLP-1 agonists as options when weight loss and strong A1C lowering are priorities.
How My Tirzepatide Journey Began
After undergoing my third spinal fusion surgery, my treatment path shifted. After long discussions about my goals (better glucose stability, less insulin, sustainable weight loss), Dr. Alka Jha, an endocrinologist at Fortis Hospital, Vasant Kunj (New Delhi), suggested I try the weekly injection. She explained how it could potentially reduce my dependence on insulin while improving both my blood sugar levels and weight. After thorough discussions and understanding the possible outcomes, I decided to begin the treatment.
In July 2025, I transitioned from semaglutide 1.7 mg weekly to Tirzepatide 2.5 mg. With the continued support of Dr. Sayem and my family physician, Dr. Mithun Chowdhury, I gradually increased the dosage, moving up carefully week by week until I reached 7.5 mg once weekly.
The real turning point came when I started 5 mg of Tirzepatide. At that stage, Dr. Mithun reduced my insulin to 8+0+6 units a day. Eventually, under Dr. Sayem’s supervision, I was able to completely stop using Humalog Mix 25 insulin in the last month—something I never thought would be possible after so many years of dependency.
My new treatment plan became much simpler:
- Metformin XR 500 mg and Empagliflozin 25 mg in the morning
- Saroglitazar 4 mg after lunch
- No diabetic medicine at night
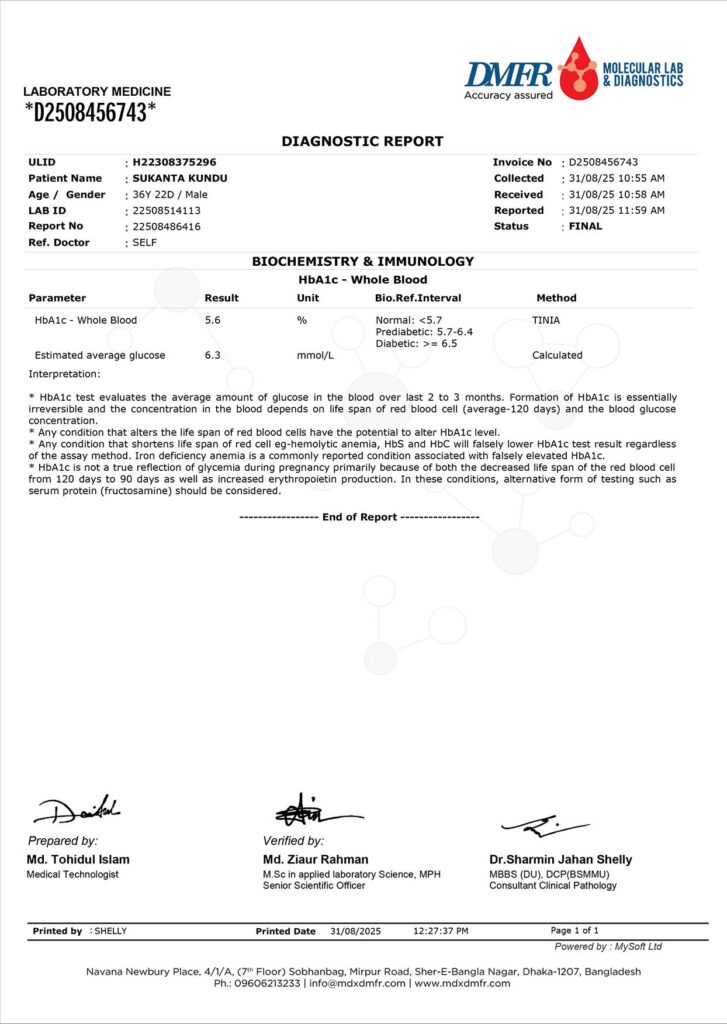
The results were remarkable. My HbA1c stabilized around 5.6%, estimated average glucose 6.3 and my current weight is 79 kg. For the first time in years, my diabetes is well controlled without insulin.
This journey hasn’t been easy, but it has been transformative. I owe my deepest gratitude to Dr. Mohammad Sayem, Dr. Mithun Chowdhury, and Dr. Alka Jha for their constant guidance, care, and encouragement. Thanks to their support, I am living a healthier, more hopeful life.
Note: These outcomes mirror what trials suggest—tirzepatide tends to lower A1C and weight and often improves triglycerides—though individual responses vary.
What I Actually Changed Day-to-Day (Beyond the Injection)
- Monitoring: I checked glucose more frequently during the first weeks to prevent lows while insulin was being reduced. (Hypoglycemia risk rises when a potent agent is combined with insulin.)
- Meals: Smaller, protein-forward meals helped minimize nausea and kept energy steady. (Guidelines advise slow dose escalation and mindful eating to limit GI side effects.)
- Hydration & electrolytes: Helped with early appetite changes and occasional mild constipation—common with incretin therapies.
- Movement & physio: Light daily activity plus physiotherapy aligned with my spine rehab (more below).
Results I’ve Noticed (and How They Compare to the Data)
| Area | What I Experienced | What Studies/Guidelines Say |
| Insulin needs | Down from 34 u/day to 12 u/day; stopped pre-dinner dose. | Potent A1C lowering with tirzepatide can enable insulin dose reductions; monitor for hypoglycemia when used with insulin. |
| A1C | 5.6% (most stable in years). | SURPASS-2: Greater A1C reduction than semaglutide 1 mg at all tirzepatide doses. |
| Weight | Steady loss, easier appetite control. | SURMOUNT-1/2025 follow-ups: ~15–22% mean weight loss at higher doses; durability out to ~3 years shown in extension data. |
| Triglycerides | Normal for the first time in years. | Meta-analyses: TG and cholesterol improve with tirzepatide; dose-response pattern. |
| Side effects | Mild early nausea, manageable with smaller meals. | Most common: GI symptoms (nausea, diarrhea, decreased appetite). Slow titration helps. |
How I Titrated (and What Labels Recommend)
Pharmaceutical labels recommend starting at 2.5 mg once weekly for 4 weeks (to allow the body to adapt), then increasing by 2.5 mg steps every 4 weeks (5 → 7.5 → 10 → 12.5 → 15 mg) as tolerated and needed for goals. Zepbound has the same escalation schedule for obesity indications. I began with a 5 mg weekly plan under close supervision because of my insulin background and ongoing rehab, with frequent checks and conservative adjustments.
Important: These medicines shouldn’t be combined with other tirzepatide-containing products or another GLP-1 at the same time.
Safety Notes I Took Seriously (From My Doctors and the Labels)
- Black-box caution: People with a personal/family history of medullary thyroid carcinoma (MTC) or MEN2 should not take tirzepatide.
- Pancreatitis, gallbladder disease, and severe GI disease are warnings; report persistent severe abdominal pain, vomiting, or jaundice.
- Dehydration risk: Because of GI effects, staying hydrated matters—especially with kidney disease risk.
- Compounded products: The ADA advises against non-FDA-approved compounded GLP-1/GIP products due to safety/quality concerns.
Managing More Than Diabetes: My Spine Story
While managing diabetes, I’ve also been coping with serious spinal issues. Over the years, I’ve undergone three spinal fusion surgeries in Delhi, including a revision spinal fusion surgery at Indian Spinal Injuries Centre (ISIC) —all led by prominent spine surgeon Dr. Neeraj Gupta and his team.
Thanks to his expertise and continued care, my spine condition has improved. Alongside medications, I’ve been actively following a physiotherapy regimen—a combination of manual therapy and active exercises. These are helping me recover from diabetic lumbosacral radiculoplexus neuropathy (DLRPN) and related nerve compression issues. Progress has been slow but steady, and I’m seeing encouraging signs of recovery.
What This Journey Taught Me
This experience has reinforced several important lessons:
- The value of trusted medical guidance: Having dedicated doctors like Dr. Alka Jha and Dr. Mithun Chowdhury made all the difference.
- The importance of listening to your body: Every change—good or bad—matters.
- Realistic expectations are essential: Tirzepatide is not a magic solution. It requires commitment, patience, and consistent monitoring.
While this medication has made a significant impact, success depends on a combination of factors—proper medical supervision, lifestyle changes, and emotional resilience.
Tips If You’re Considering Tirzepatide (From My Lived Experience)
If you’re thinking about trying Tirzepatide, here’s what I’d recommend:
- Consult your doctors thoroughly: Discuss your full medical history and all current conditions.
- Start with the labels & standards: Confirm you’re a good candidate and understand titration, side effects, and red flags.
- Plan insulin reductions early: If you’re on insulin, schedule proactive dose-review windows as A1C falls. Finding the right balance may take time.
- Use “GI-friendly” routines: Small, protein-rich meals; avoid very fatty meals on a short day; hydrate.
- Expect variability: Not everyone loses the same amount of weight or gets the same A1C drop—individual response varies, and that’s normal.
- Stick with safe sources: Avoid compounded versions unless clearly verified and clinically necessary.
- Be transparent: Share any side effects or concerns right away.
- Track your blood sugar regularly: Keep close watch, especially in the early weeks.
- Stay committed to lifestyle changes: Diet, exercise, and physiotherapy can amplify the medication’s benefits.
- Be patient and kind to yourself: Some days will be harder than others—but consistency matters.
Final Thoughts
My decade-long journey with diabetes has had its fair share of highs and lows. But Tirzepatide has opened a new, hopeful chapter. With better blood sugar control, reduced insulin use, and improved lab results, I finally feel like I’m regaining control over my health.
Of course, the road hasn’t been easy—with spinal surgeries and nerve complications adding to the challenge. But thanks to the unwavering support from my doctors, a tailored physiotherapy plan, and the right medications, I feel more optimistic than ever.
If you’re managing type 2 diabetes and exploring new treatment options, I hope my experience offers some insight and encouragement. Tirzepatide isn’t a cure, but in the right context, it can be a powerful tool in your health journey—just as it has been in mine.
Thank you for taking the time to read about my journey. I hope it helps you or someone you care about to make informed, thoughtful decisions in managing chronic conditions like diabetes. Open communication with your healthcare providers and a patient, persistent mindset can truly make a difference.