As the world continues to grapple with the aftermath of the COVID-19 pandemic, a new respiratory threat has emerged in China, causing concern among global health authorities. Human metapneumovirus (HMPV), a long-known but often overlooked respiratory pathogen, has recently seen a surge in cases, particularly among children.
This development has sparked comparisons to the early days of the COVID-19 outbreak, raising questions about the potential for another global health crisis.While both HMPV and SARS-CoV-2 (the virus responsible for COVID-19) are respiratory pathogens capable of causing significant illness, they differ in many crucial aspects.
This article aims to provide a comprehensive comparison of HMPV vs COVID-19, examining their similarities, differences, and the implications for public health.
What is HMPV
Human metapneumovirus (HMPV) is a respiratory virus that has been circulating globally for decades, yet it remains relatively unknown to the general public. First discovered in 2001 in the Netherlands, HMPV has been found to be a common cause of respiratory infections, particularly in young children, older adults, and immunocompromised individuals
Discovery and History of HMPV
HMPV’s discovery in 2001 was a significant milestone in virology. Although it was newly identified at the time, serological studies demonstrated that this pathogen had been circulating in the Netherlands since at least 1958.
This finding suggests that HMPV had been causing respiratory infections for many years before its official discovery, often misdiagnosed or overlooked due to its similarity to other respiratory viruses.
Transmission and Seasonality of HMPV
HMPV spreads primarily through respiratory droplets when an infected person coughs, sneezes, or talks. It can also spread through close personal contact, such as touching or shaking hands, and by touching surfaces contaminated with the virus and then touching one’s mouth, nose, or eyes.
One of the key characteristics of HMPV is its distinct seasonal pattern. In temperate climates, HMPV circulation typically begins in winter and lasts until or through spring.
This seasonality is similar to other respiratory viruses like influenza and respiratory syncytial virus (RSV), often leading to concurrent circulation of these pathogens during the respiratory virus season.
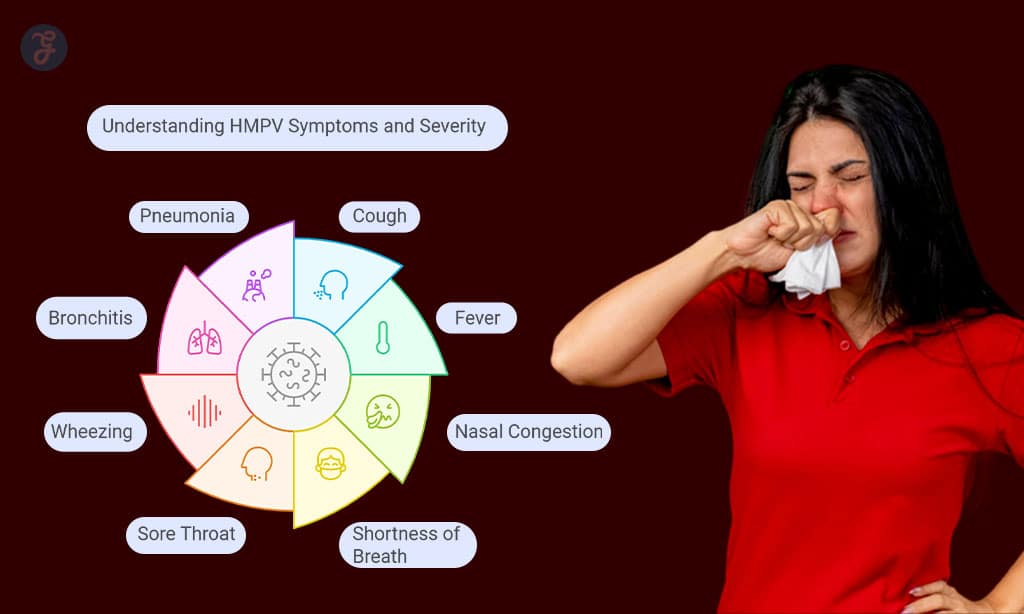
HMPV: Common Symptoms and Severity
HMPV infections can range from mild to severe, with symptoms often mimicking those of other respiratory infections. Common symptoms include:
- Cough
- Fever
- Nasal congestion
- Shortness of breath
- Sore throat
- Wheezing (in severe cases)
While most HMPV infections result in mild, cold-like symptoms, the virus can cause more severe illnesses, particularly in vulnerable populations. These can include bronchitis, pneumonia, and exacerbations of existing conditions like asthma or chronic obstructive pulmonary disease (COPD).
The severity of HMPV infections can vary significantly depending on the individual’s age and health status. Children under five years old, especially infants, are at higher risk for severe infections. Similarly, older adults (particularly those over 65) and individuals with weakened immune systems or chronic respiratory conditions are more vulnerable to complications from HMPV.
HMPV vs COVID-19: Key Similarities
While HMPV and SARS-CoV-2 are distinct viruses belonging to different viral families, they share several important similarities that have contributed to the recent comparisons between the two.
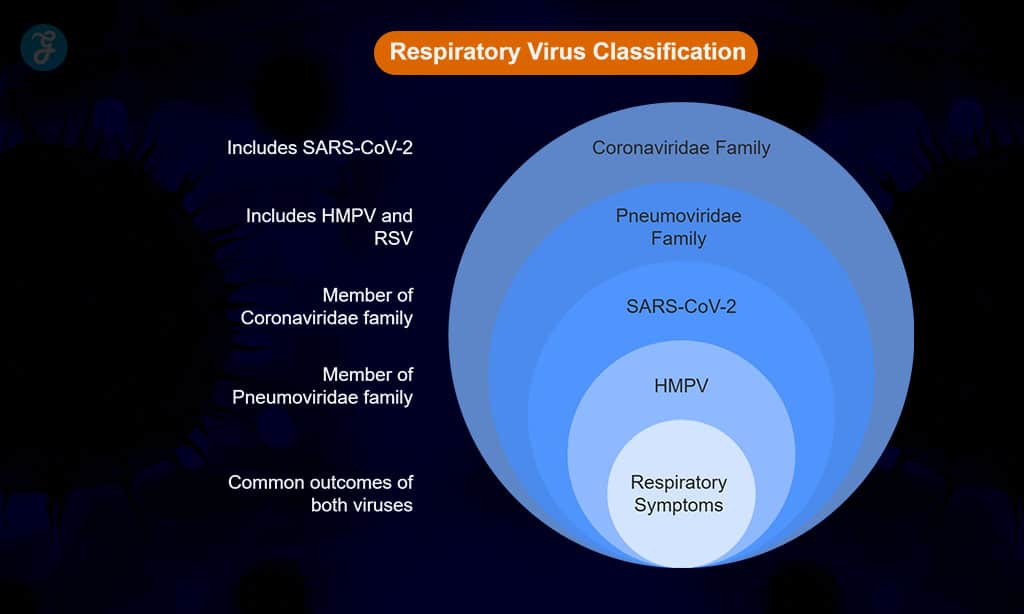
Respiratory Virus Classification
Both HMPV and SARS-CoV-2 are classified as respiratory viruses, meaning they primarily target the respiratory system. HMPV belongs to the Pneumoviridae family, which also includes respiratory syncytial virus (RSV). SARS-CoV-2, on the other hand, is a member of the Coronaviridae family.
Despite their different classifications, both viruses can cause a range of respiratory symptoms, from mild upper respiratory tract infections to severe pneumonia.
HMPV vs COVID-19: Transmission Methods
The transmission methods for HMPV and SARS-CoV-2 are strikingly similar. Both viruses spread primarily through respiratory droplets expelled when an infected person coughs, sneezes, or talks. Close personal contact, such as touching or shaking hands with an infected individual, can also lead to transmission.
Additionally, both viruses can survive on surfaces for some time, allowing for indirect transmission when a person touches a contaminated surface and then touches their mouth, nose, or eyes.
Vulnerable Populations
Another significant similarity between HMPV and COVID-19 is the populations most vulnerable to severe infections. For both viruses, the following groups are at higher risk:
- Young children, especially those under 5 years old
- Older adults, particularly those over 65
- Individuals with weakened immune systems
- People with underlying chronic medical conditions, especially respiratory diseases like asthma or COPD
This overlap in vulnerable populations means that public health measures aimed at protecting these groups can be effective against both viruses.
HMPV vs COVID-19: Overlapping Symptoms
HMPV and COVID-19 share many common symptoms, which can make initial diagnosis challenging without specific testing. Both infections can cause:
- Fever
- Cough
- Shortness of breath
- Fatigue
- Sore throat
- Nasal congestion
The similarity in symptoms has led to increased vigilance and testing in healthcare settings, particularly during the winter months when both viruses are more prevalent.
HMPV vs COVID-19: Critical Differences
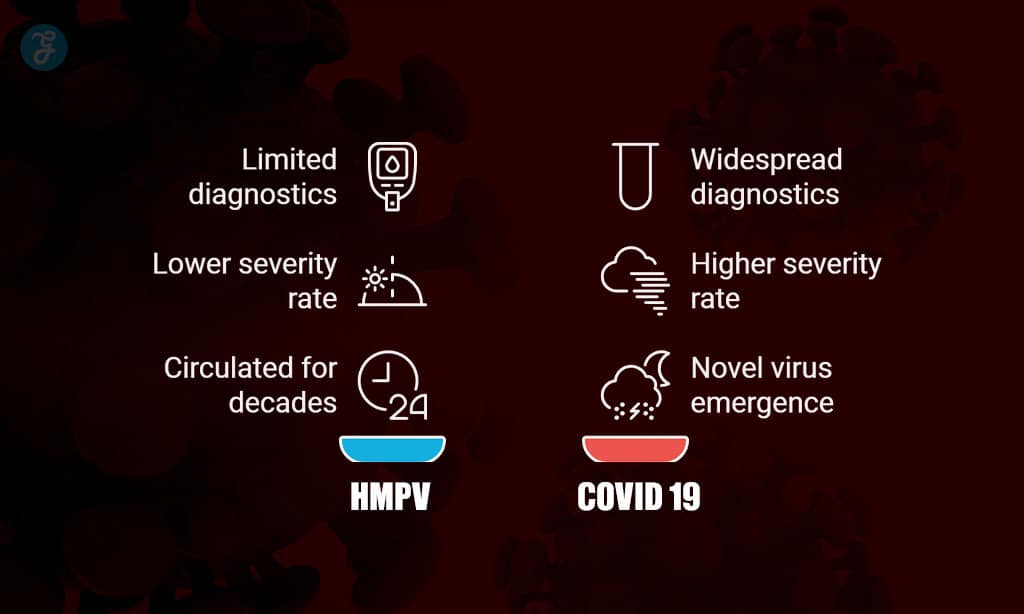
Despite their similarities, HMPV and COVID-19 have several critical differences that impact their spread, severity, and management.
Novelty and Population Immunity
One of the most significant differences between HMPV and COVID-19 lies in their novelty and the population’s existing immunity. HMPV has been circulating in human populations for decades, with studies showing that nearly all children have been exposed to the virus by the age of 5.
This long-term circulation means that most adults have some level of immunity to HMPV, even if they can still be reinfected.In contrast, SARS-CoV-2 emerged as a novel virus in late 2019, meaning the global population had no pre-existing immunity. This lack of immunity contributed to the rapid spread of COVID-19 and its severe impact on global health systems.
Severity and Complications
While both viruses can cause severe illness, COVID-19 has demonstrated a higher potential for severe complications and mortality, particularly in its initial waves before widespread vaccination. COVID-19 can lead to a broader range of systemic complications, including:
- Acute respiratory distress syndrome (ARDS)
- Multiorgan failure
- Blood clotting disorders
- Long-term neurological symptoms (Long COVID)
HMPV, while capable of causing severe respiratory illness, typically results in milder symptoms and has a lower mortality rate. Severe cases of HMPV are generally limited to respiratory complications such as pneumonia or bronchiolitis, particularly in high-risk groups.
Diagnostic Challenges
The diagnostic approach for HMPV and COVID-19 differs significantly. COVID-19 testing became widely available and routine during the pandemic, with rapid antigen tests and PCR tests specifically designed to detect SARS-CoV-2. In contrast, HMPV testing is less common and often requires specific molecular diagnostic techniques that may not be routinely available in all healthcare settings.
This difference in diagnostic availability and approach can lead to underreporting of HMPV cases compared to COVID-19, potentially masking the true prevalence of HMPV infections.
Available Treatments and Vaccines
Perhaps the most critical difference between HMPV and COVID-19 lies in the available treatments and preventive measures. The global response to COVID-19 led to the rapid development of multiple effective vaccines and antiviral treatments. As of January 2025, several COVID-19 vaccines are widely available, and antiviral medications like remdesivir have shown efficacy in treating severe cases.
In contrast, there is currently no specific antiviral treatment or vaccine available for HMPV. Management of HMPV infections primarily focuses on supportive care, such as managing symptoms and providing respiratory support in severe cases.
This lack of specific interventions highlights the need for continued research and development in the field of HMPV therapeutics.
Public Health Implications
The recent surge in HMPV cases, particularly in China, has raised concerns about its potential impact on public health systems globally. Understanding the implications of HMPV in the context of the ongoing management of COVID-19 is crucial for effective public health planning and response.
Current Global Spread of HMPV
While HMPV has been circulating globally for decades, the recent outbreak in China has brought renewed attention to this virus. Reports indicate a significant increase in HMPV cases, particularly among children under the age of 14, with many requiring hospitalization due to the severity of their symptoms.
This surge has occurred during the typical peak season for HMPV in the northern hemisphere, highlighting the importance of seasonal awareness in managing respiratory infections.The global spread of HMPV is difficult to quantify precisely due to variations in testing and reporting practices across different countries.
However, surveillance data from the U.S. Centers for Disease Control and Prevention (CDC) shows that HMPV activity typically peaks during late winter and spring in temperate climates. The current outbreak in China may indicate a potential for increased HMPV activity in other regions as well.
Healthcare System Impact
The impact of HMPV on healthcare systems can be significant, particularly when cases surge during peak seasons. While HMPV infections are generally less severe than COVID-19, they can still lead to hospitalizations, especially among vulnerable populations.
A study published in the journal Immunity in 2021 found that approximately 5% to 25% of acute pediatric lower respiratory tract infections are associated with HMPV.
The potential for concurrent circulation of HMPV, COVID-19, and other respiratory viruses like influenza and RSV poses a challenge for healthcare systems. This “multi-demic” scenario can lead to increased strain on hospital resources, particularly pediatric and respiratory care units. Healthcare providers must be prepared to differentiate between these infections and manage potential co-infections.
Surveillance and Monitoring Efforts
The COVID-19 pandemic has significantly enhanced global surveillance and monitoring capabilities for respiratory viruses. These improved systems are now being leveraged to track HMPV and other respiratory pathogens more effectively. In the United States, the CDC’s National Respiratory and Enteric Virus Surveillance System (NREVSS) monitors HMPV activity alongside other respiratory viruses.
Enhanced surveillance is crucial for early detection of outbreaks and unusual patterns of viral spread. It also provides valuable data for researchers studying the epidemiology of HMPV and its interactions with other respiratory pathogens. Continued investment in these surveillance systems will be essential for managing future respiratory disease threats.
Lessons Learned from COVID-19
The global response to the COVID-19 pandemic has provided valuable lessons that can be applied to the management of HMPV and other respiratory viruses. These lessons have implications for pandemic preparedness, public health communication, and global cooperation in disease management.
Improved Pandemic Preparedness
The COVID-19 pandemic exposed gaps in global pandemic preparedness but also led to significant improvements in response capabilities. Key lessons that can be applied to HMPV and other emerging threats include:
- Rapid diagnostic development: The quick development and deployment of COVID-19 tests demonstrated the importance of flexible diagnostic platforms that can be quickly adapted to new pathogens.
- Vaccine research and development: The unprecedented speed of COVID-19 vaccine development has paved the way for faster responses to future viral threats, potentially benefiting HMPV vaccine research.
- Supply chain resilience: Experiences with personal protective equipment (PPE) shortages during the early stages of the COVID-19 pandemic have led to improved stockpiling and supply chain management strategies.
- Surge capacity planning: Healthcare systems have developed better strategies for rapidly expanding capacity to handle patient surges, which can be applied to HMPV outbreaks.
Enhanced Public Health Communication
The COVID-19 pandemic highlighted the critical importance of clear, consistent, and transparent public health communication. Lessons that can be applied to HMPV and other respiratory viruses include:
- Consistent messaging: Providing clear, science-based information to the public helps combat misinformation and promotes adherence to preventive measures.
- Risk communication: Effectively communicating the risks associated with respiratory viruses without causing undue panic is crucial for maintaining public trust and cooperation.
- Digital platforms: Leveraging social media and other digital platforms for rapid dissemination of public health information has proven effective and can be applied to HMPV awareness campaigns.
- Cultural sensitivity: Tailoring communication strategies to different cultural contexts and addressing community-specific concerns improves the effectiveness of public health messaging.
Importance of Global Cooperation
The COVID-19 pandemic underscored the interconnectedness of global health and the need for international cooperation in managing infectious diseases. Lessons that can be applied to HMPV and future health threats include:
- Data sharing: Rapid and transparent sharing of epidemiological data and genetic sequences facilitates global monitoring and research efforts.
- Collaborative research: International collaboration in research and development accelerates the discovery of treatments and vaccines.
- Equitable access: Ensuring equitable global access to diagnostics, treatments, and vaccines is crucial for effective disease control.
- Coordinated response: Aligning public health measures across borders helps contain the spread of respiratory viruses more effectively.
Prevention and Management Strategies
Effective prevention and management of HMPV infections draw on strategies that have proven successful against COVID-19 and other respiratory viruses. These approaches focus on personal hygiene, vaccination efforts, and healthcare system readiness.
Personal Hygiene Measures
Many of the personal hygiene measures promoted during the COVID-19 pandemic are equally effective against HMPV. These include:
- Hand hygiene: Regular handwashing with soap and water or using alcohol-based hand sanitizers helps prevent the spread of HMPV and other respiratory viruses.
- Respiratory etiquette: Covering the mouth and nose when coughing or sneezing, preferably with a tissue or the elbow, reduces the spread of respiratory droplets.
- Mask-wearing: While not as universally recommended as during the height of the COVID-19 pandemic, mask-wearing can still be beneficial, particularly for high-risk individuals or in healthcare settings during HMPV season.
- Surface cleaning: Regular cleaning and disinfection of frequently touched surfaces can help reduce the risk of indirect transmission.
- Social distancing: Maintaining physical distance from individuals who are sick, especially during peak HMPV season, can help reduce transmission.
Vaccination Efforts
While there is currently no vaccine available for HMPV, the lessons learned from COVID-19 vaccination campaigns can inform future efforts:
- Vaccine development: Ongoing research into HMPV vaccines can benefit from the accelerated development processes used for COVID-19 vaccines.
- Targeted vaccination: When an HMPV vaccine becomes available, prioritizing high-risk groups, such as young children and older adults, will be crucial.
- Public education: Building on COVID-19 vaccine education efforts to promote understanding and acceptance of new vaccines will be important for HMPV vaccination campaigns.
- Integration with existing programs: Incorporating HMPV vaccination into existing immunization programs, such as annual flu shot campaigns, could improve uptake.
Healthcare System Readiness
Preparing healthcare systems to manage HMPV outbreaks alongside other respiratory infections is crucial:
- Diagnostic capacity: Expanding and maintaining capacity for rapid, accurate diagnosis of HMPV and other respiratory pathogens is essential for effective management.
- Treatment protocols: Developing and updating treatment protocols for HMPV, particularly for severe cases, ensures consistent and effective patient care.
- Resource allocation: Flexible resource allocation strategies, including staff and equipment, help healthcare systems respond to seasonal surges in respiratory infections.
- Telemedicine: Leveraging telemedicine platforms for initial assessments and follow-up care can help manage patient volumes during peak seasons.
- Infection control: Maintaining robust infection control practices in healthcare settings helps prevent the spread of HMPV and other respiratory viruses among patients and staff.
HMPV vs COVID-19: Future Outlook
As we continue to navigate the complex landscape of respiratory viruses, including HMPV and COVID-19, several key areas will shape the future of prevention, treatment, and management.
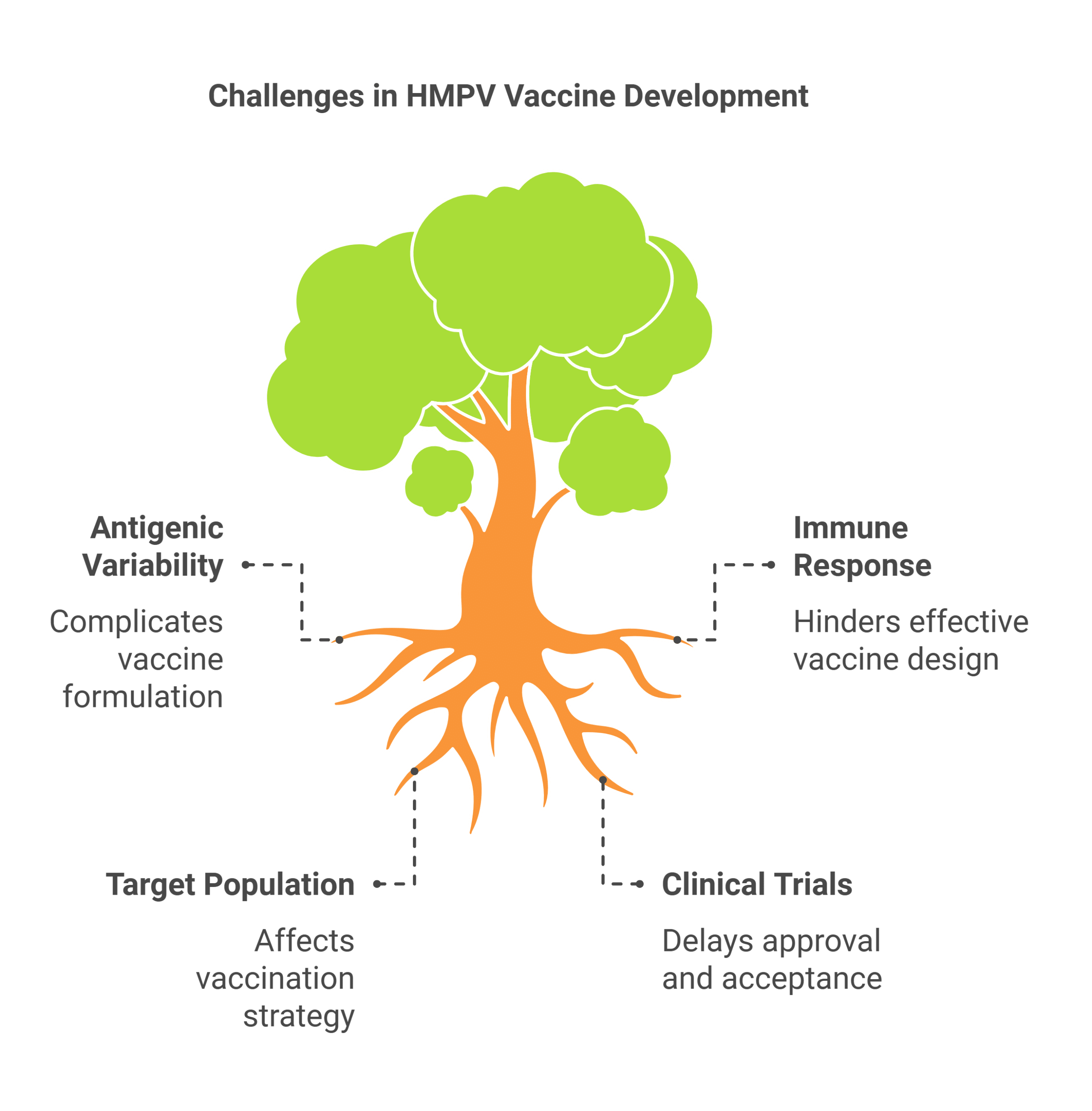
Potential for HMPV Vaccine Development
The success of COVID-19 vaccine development has reinvigorated interest in vaccines for other respiratory viruses, including HMPV. While there is currently no approved vaccine for HMPV, research is ongoing. The challenges in developing an HMPV vaccine include:
- Antigenic variability: Like many respiratory viruses, HMPV has multiple strains, which can complicate vaccine development.
- Immune response: Understanding the long-term immune response to HMPV infection is crucial for developing effective vaccines.
- Target population: Determining the optimal age for vaccination, particularly for young children who are most at risk, will be important for vaccine implementation.
- Clinical trials: Conducting large-scale clinical trials to demonstrate safety and efficacy will be crucial for vaccine approval and public acceptance.
Despite these challenges, the advancements in vaccine technology spurred by the COVID-19 pandemic, such as mRNA platforms, may accelerate HMPV vaccine development. Successful development of an HMPV vaccine could significantly reduce the burden of respiratory infections, particularly in vulnerable populations.
HMPV vs COVID-19: Ongoing Research and Surveillance
The heightened awareness of respiratory viruses following the COVID-19 pandemic has led to increased research and surveillance efforts for other pathogens like HMPV. Key areas of focus include:
- Epidemiological studies: Ongoing research to better understand the prevalence, transmission patterns, and risk factors associated with HMPV infections.
- Genetic sequencing: Continued monitoring of HMPV genetic diversity to track the emergence of new variants and inform vaccine development.
- Pathogenesis research: Further studies on how HMPV causes disease, particularly in severe cases, to guide the development of targeted treatments.
- Diagnostic improvements: Development of more sensitive and specific diagnostic tests for HMPV, potentially including multiplex assays that can detect multiple respiratory pathogens simultaneously.
- Treatment research: Exploration of antiviral therapies and other treatment modalities specific to HMPV infections.
Enhanced surveillance systems, such as those implemented during the COVID-19 pandemic, will play a crucial role in monitoring HMPV activity and detecting unusual outbreaks. Integration of HMPV surveillance into existing respiratory virus monitoring programs will provide a more comprehensive picture of respiratory disease burden.
The Role of Climate Change and Urbanization
Environmental factors, particularly climate change and increasing urbanization, may impact the future spread and severity of respiratory viruses like HMPV:
- Altered seasonality: Climate change may affect the traditional seasonality of respiratory viruses, potentially leading to longer or shifted peak seasons for HMPV.
- Geographic spread: Changes in temperature and precipitation patterns could alter the geographic distribution of HMPV and other respiratory pathogens.
- Increased transmission: Higher population densities in urban areas may facilitate the rapid spread of respiratory viruses, including HMPV.
- Air quality: Deteriorating air quality in urban areas may increase susceptibility to respiratory infections, potentially exacerbating the impact of HMPV.
Understanding these environmental factors will be crucial for predicting and managing future HMPV outbreaks.
Takeaways
While Human metapneumovirus (HMPV) has long existed as a respiratory pathogen, its recent surge in cases underscores the importance of heightened awareness and proactive public health measures. Despite its similarities to COVID-19 in transmission methods and vulnerable populations, HMPV typically causes less severe illness but remains a significant concern for children, older adults, and immunocompromised individuals.
The lessons learned from the COVID-19 pandemic—such as rapid diagnostic development, enhanced surveillance, and improved public health communication—can be effectively applied to managing HMPV.
Moving forward, continued research into vaccines and treatments, coupled with robust healthcare preparedness, will be critical to mitigating the impact of HMPV and other emerging respiratory threats.