A groundbreaking set of studies has revealed that sodium-glucose co-transporter-2 (SGLT2) inhibitors — a class of drugs initially designed to treat type 2 diabetes — provide consistent and significant protection for both the kidneys and the heart across a remarkably broad patient population. The findings were presented at the American Society of Nephrology’s Kidney Week and simultaneously published in two companion papers in JAMA. Together, the data represent the largest and most comprehensive evaluation yet of SGLT2 inhibitors, involving more than 70,000 participants across ten major randomized controlled trials.
The research, conducted by the SGLT2 Inhibitor Meta-Analysis Cardio-Renal Trialists’ Consortium (SMART-C) and led by scientists from The George Institute for Global Health, delivers robust evidence that these medications offer powerful benefits not only for people with diabetes but also for those suffering from chronic kidney disease (CKD) and heart failure — even if they do not have diabetes.
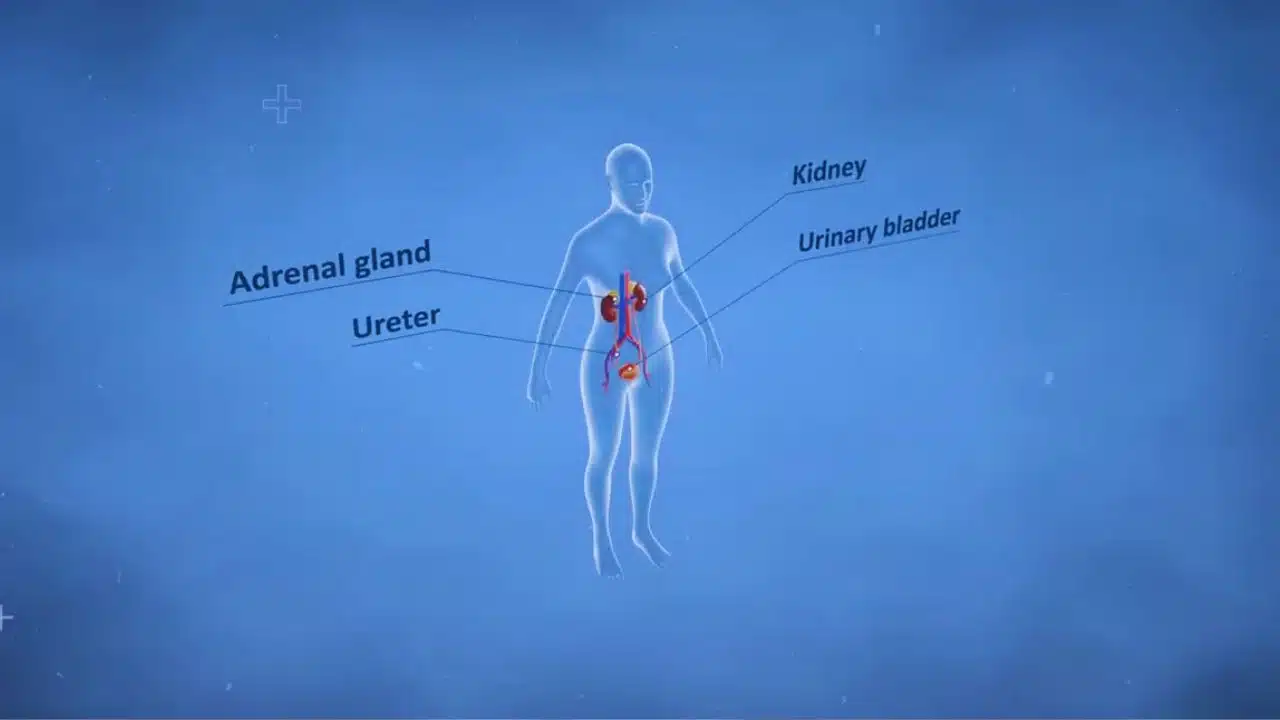
SGLT2 inhibitors, which include well-known drugs such as dapagliflozin, empagliflozin, and canagliflozin, work by reducing the reabsorption of glucose in the kidneys, leading to lower blood sugar levels. However, clinical trials over the past decade have hinted at much broader effects, including reduced cardiovascular deaths, fewer hospitalizations for heart failure, and a slower decline in kidney function. The new analyses confirm that these benefits are consistent across almost every type of patient studied, marking a major advance in preventive and therapeutic nephrology.
The studies addressed one of the field’s most debated questions: whether SGLT2 inhibitors remain effective in people with advanced CKD — whose kidney function is already severely impaired — and in those with minimal or no albuminuria (a low level of protein in the urine, often seen in the early stages of kidney damage). Until now, evidence for these groups was limited, and many physicians were uncertain about prescribing the drugs outside traditional diabetes or albuminuria thresholds.
Landmark Findings Across All Kidney and Heart Risk Groups
In the first analysis, SMART-C researchers combined detailed data from tens of thousands of trial participants to evaluate kidney outcomes. They found that SGLT2 inhibitors reduced the risk of CKD progression by an impressive 38 percent compared with placebo. This benefit was remarkably stable regardless of the patient’s baseline kidney function or degree of proteinuria. Whether a person had relatively normal kidney filtration rates or was already in stage 4 CKD (with an estimated glomerular filtration rate, or eGFR, below 30 mL/min/1.73 m²), the relative advantage of taking an SGLT2 inhibitor remained strong.
The analysis also showed that these drugs slowed the annual decline in eGFR — a key indicator of kidney function — by 51 percent compared to placebo. In practical terms, that means patients maintained healthier kidney performance for much longer periods, delaying or even preventing the need for dialysis or kidney transplantation. The consistency of this effect across all subgroups, including those with minimal albumin in their urine, is one of the most significant revelations from the study.
In the second companion paper, researchers assessed the impact of SGLT2 inhibitors on both cardiovascular and renal outcomes, this time focusing on differences by diabetes status and albuminuria level. The results were striking: the benefits extended equally to people with and without diabetes. Hospitalizations for heart failure — one of the leading causes of death and medical costs worldwide — were reduced by nearly one-third among participants with diabetes and by roughly one-quarter among those without it.
The safety data were equally reassuring. The risk of serious side effects was very low, and overall, the positive outcomes on kidney and heart health far outweighed any potential adverse events. These findings dismantle earlier assumptions that SGLT2 inhibitors should be limited to diabetic patients or those with high levels of proteinuria. Instead, the data point toward universal protective effects for the kidneys and cardiovascular system, regardless of baseline disease characteristics.
Associate Professor Brendon Neuen, Renal and Metabolic Program Lead at The George Institute for Global Health and lead author of one of the studies, described the findings as “the strongest evidence yet to support widespread use of SGLT2 inhibitors in people with chronic kidney disease.” He emphasized that these drugs now stand as a cornerstone of preventive treatment — a single intervention capable of reducing the risks of kidney failure, hospitalization, and premature death across a vast population of at-risk individuals.
Neuen also noted that the studies support simplifying and expanding treatment guidelines to encourage much broader use of SGLT2 inhibitors, including among patients previously excluded from therapy. He called this “a once-in-a-generation opportunity to transform care for millions of people living with or at risk of developing kidney disease.”
The significance of this research cannot be overstated. Chronic kidney disease currently affects about one in ten people globally — roughly 850 million men and women — and is a leading cause of death and disability worldwide. The burden is especially high in low- and middle-income countries, where diagnosis often comes late and access to effective therapy remains limited. SGLT2 inhibitors could offer an affordable, scalable solution to mitigate this enormous health challenge once they become widely available in generic forms over the next few years.
Transforming Global Care for Chronic Kidney Disease
These new meta-analyses represent a turning point in the global management of CKD and related cardiovascular conditions. By confirming that the benefits of SGLT2 inhibitors span nearly every patient category, researchers have laid the groundwork for a major revision of current clinical practice guidelines. The evidence now supports prescribing these medications broadly — not only to people with type 2 diabetes but to anyone with kidney impairment, heart failure, or even early markers of kidney dysfunction.
The implications are profound. For patients, the findings promise longer, healthier lives with fewer hospitalizations, less need for dialysis, and reduced cardiovascular risk. For clinicians, they offer a simplified and evidence-based pathway for treatment decisions: instead of waiting for advanced disease or high protein levels to develop, SGLT2 inhibitors can be introduced earlier as a preventive measure. And for health systems, especially in resource-limited settings, this could translate into substantial reductions in long-term costs related to dialysis, transplants, and heart-failure management.
As more affordable generic versions of these medicines enter the market, experts anticipate a rapid expansion in accessibility worldwide. Public health organizations and policymakers are being urged to prioritize these drugs in essential-medicine lists, particularly in countries facing soaring rates of diabetes and kidney disease.
According to researchers at The George Institute, the global healthcare community now faces an unprecedented opportunity: to implement these findings at scale and drastically reduce the burden of CKD. If governments, insurers, and health providers act quickly, SGLT2 inhibitors could prevent millions of cases of kidney failure and cardiovascular death in the coming decade.
In conclusion, the SMART-C collaboration has provided the most definitive proof to date that SGLT2 inhibitors deliver consistent, meaningful cardio-renal protection across all key patient groups — diabetic or non-diabetic, early-stage or advanced CKD, high or low albuminuria. With the data now beyond dispute, attention must shift from research to implementation. As Associate Professor Neuen aptly summarized, “We have the evidence, we have the tools — now it’s time to use them to change lives.”
The Information is Collected from George Institute and News Medical.