Depression can change how a person feels about food. Some people stop feeling hungry, while others may eat more. Different types of depression cause these changes in different ways. Typical depression often brings a loss of appetite, while atypical depression can cause people to eat more. Atypical depression affects between fifteen and thirty-six percent of people diagnosed with depression.
Some people with depression feel tired most of the time. Even simple tasks like making a meal can feel hard. Others do not have an interest in things they used to enjoy, including cooking or eating. Anxiety is also common in depression and can cause stomach pain, nausea, or diarrhea. These symptoms can make eating food unpleasant or even painful.
For many, depression brings low energy. When a person is tired, they may skip meals or stop paying attention to their eating habits. With less food, energy drops even more. This cycle can make depression worse.
Why Appetite Drops During Depression
Multiple reasons explain why depression affects eating. One reason is emotional. People may feel sad, worthless, or hopeless. When feeling this way, it may be easy to stop caring about meals or forget to eat at all. Another reason is physical. Some antidepressant medications cause a loss of appetite or stomach discomfort, making it harder to stick to a regular meal schedule.
Negative thoughts are also common. A person might believe that eating does not matter, or that they do not deserve to feel better. This thinking makes it even harder to care for basic needs.
Gastrointestinal symptoms linked with depression, like pain or nausea, can stop a person from wanting food. Along with changes in sleep, these symptoms contribute to weight loss or malnutrition. When someone loses weight or develops health problems due to poor nutrition, depression often worsens.
Building a Plan: Steps That Work
No single approach works for everyone, but certain steps can support appetite and nutrition. Keeping a meal schedule can help. Eating small meals on a regular basis can feel less overwhelming than preparing large portions. Choosing simple or familiar foods can also help when interest in eating is low.
Keeping ready-to-eat foods on hand makes meals easier when energy is scarce. Protein shakes, cut vegetables, bananas, or yogurt are a few examples.
Incorporating food into small routines can make eating feel more manageable. Some people find success by linking eating with another activity, such as having a snack during a television show or after a walk.
Making mealtime social, such as eating with family or friends, can provide support. Even virtual meals with someone on a video call can help.
Routine is important. Eating and sleeping at regular times provides some structure, which supports both mood and energy levels. A reliable sleep schedule can also reduce feelings of tiredness and give a person the stamina to prepare and eat food.
Unexpected Triggers That May Influence Appetite
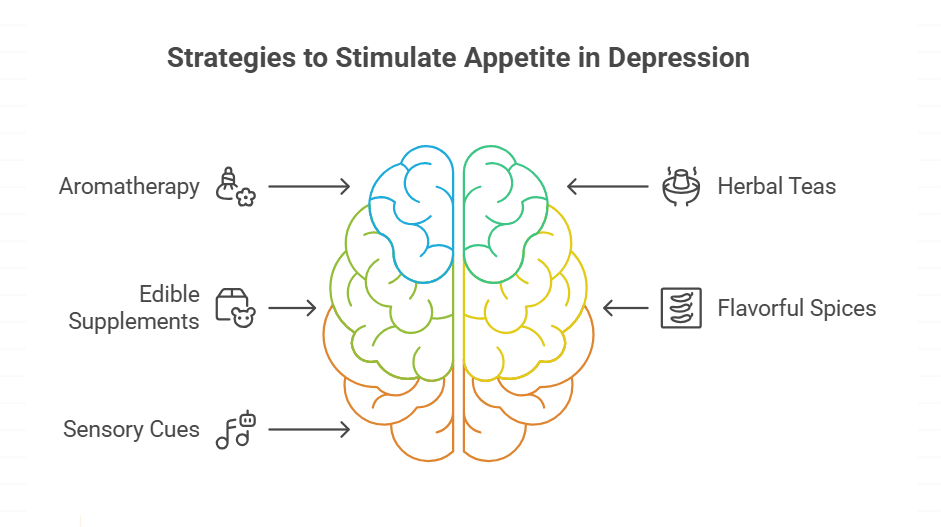
Different techniques or tools can prompt changes in appetite for those with depression. Aromatherapy with peppermint oil, herbal teas such as chamomile, or products infused with cannabidiol or tetrahydrocannabinol have all been explored for their effects. For example, Koi Delta 8 Gummies are one of several edible supplements that some people consider, alongside herbal blends and prescribed appetite stimulants, when conventional food seems less appealing.
It is important to recognize that results vary from person to person. While one person might respond to herbal extracts or edible products, another might prefer flavorful spices or sensory cues, such as music or pleasant scents, to stimulate hunger. These strategies can be used in combination with other dietary approaches or sleep schedule adjustments.
Caring for Mental and Physical Health Together
It is common for people with depression to skip meals or leave them unfinished. This creates a pattern where poor nutrition makes depression worse, and in turn, lower mood makes eating even harder. Breaking this cycle starts with small, consistent steps.
Trying to regain old pleasures is another approach. Some people benefit when they return to activities they once liked, even if it feels hard at first. Cooking a simple meal, trying a new fruit, or eating outside can offer small rewards and support appetite.
Professional support is also available. Many psychological treatments and medicines help manage depression by targeting its causes. In some cases, medicines can directly stimulate appetite or address physical symptoms like nausea. Early treatment is linked to better outcomes, so reaching out for help as soon as possible is recommended.
Prevention programs also show results. These programs aim to identify early signs of depression and address them before they affect eating or health.
Key Points About Nutrition and Recovery
Keeping up with basic nutrition supports both mental and physical health. Some tips include:
- Choose foods that are easy to eat if cooking is difficult.
- Store snacks in places that are easy to reach, so eating does not feel like a chore.
- Drink water throughout the day, since dehydration can affect mood and appetite.
- Limit alcohol, since it often makes depression symptoms worse.
If swallowing food seems difficult or appetite does not come back, consider speaking to a health professional. Medical providers may suggest supplements or appetite stimulants. Monitoring weight, energy, and meal patterns can help guide treatment decisions.
The Role of Routine and Environment
Setting up the environment can make eating easier. Some people play music or use pleasant scents to help set a mood that supports eating. Preparing food ahead of time or arranging to eat with someone else can also help bring structure to the day.
Visual cues, like keeping fruit on the counter or snacks in view, make it easier to remember to eat. Using a calendar to mark meal times can be helpful, especially when symptoms make it hard to keep track of time.
Getting sunlight in the morning or spending a few minutes outside can increase energy and encourage hunger. Light exposure ties in with sleep, which is linked with mood and appetite.
Exploring Treatment with Care
Many medicines for depression can help mood improve over time, but some do cause stomach problems at first. Not everyone reacts to medicines in the same way, so communication with health professionals is important. If a medicine upsets the stomach or reduces hunger, let the provider know, as alternatives may be available.
Psychological therapies can also improve how a person thinks about food and self-care. Counseling can address negative beliefs and teach small steps to rebuild healthy patterns.
Supporting a Balanced Diet
Depression can make food lose its appeal, but the body still needs nutrients. Eating a mix of proteins, fruits, and grains helps the body function and repair itself.
If full meals seem overwhelming, try focusing on snacks or drinks with high nutrition. Some people do better with small bites spread throughout the day rather than forcing large meals.
Asking for help, such as a friend dropping off groceries or meals, can remove obstacles. Community programs or meal delivery services might also help keep nutrition on track when energy or motivation drops.
Summary
Depression changes how people relate to food, appetite, and nutrition. Several strategies, including small regular meals, easy foods, structured routines, and supportive environments, can support appetite. Medical and psychological treatments also play a role. Keeping nutrition in focus helps support the body and mind, even when appetite is low.