In a medical achievement that could redefine how stroke patients receive emergency care, doctors from Scotland and the United States have successfully completed what is believed to be the world’s first robot-assisted remote stroke surgery on a human body. The pioneering procedure, known as a remote mechanical thrombectomy, involved removing blood clots from the brain using robotic precision — but with the surgeon located thousands of miles away.
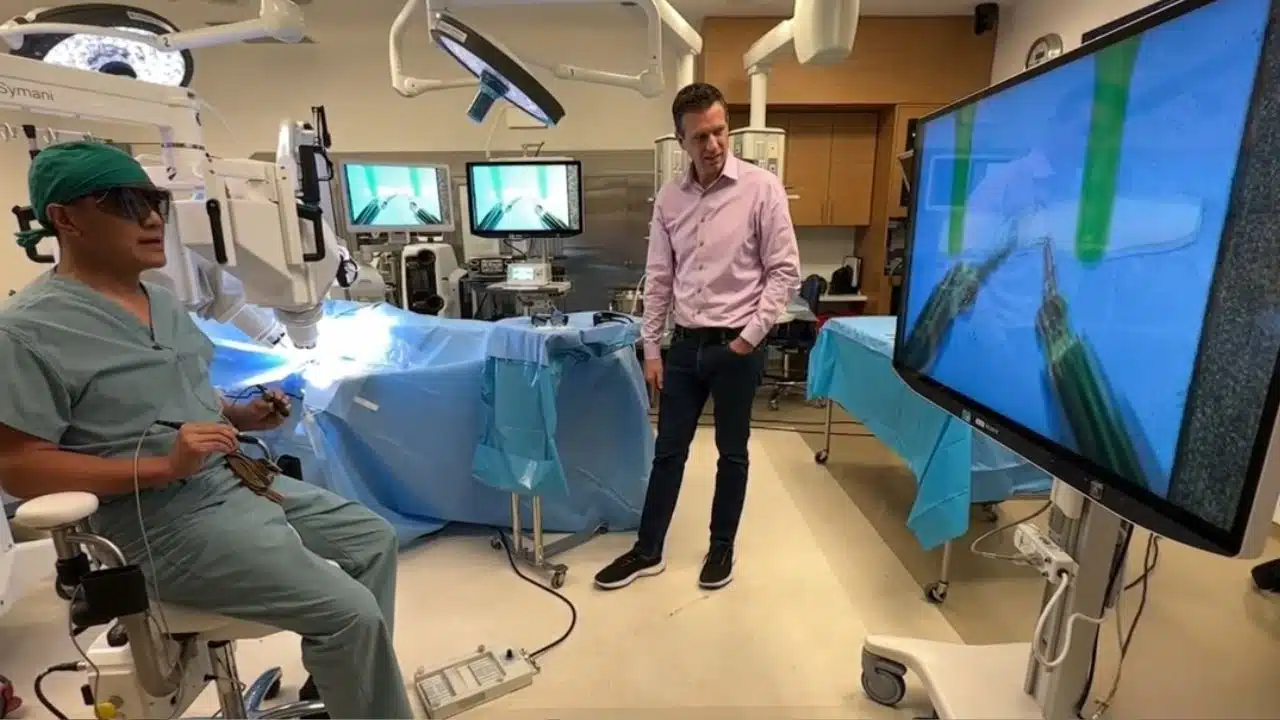
The groundbreaking experiment took place between Ninewells Hospital in Dundee, Scotland, and a medical facility in Florida, USA. Professor Iris Grunwald, a world-renowned interventional neuroradiologist from the University of Dundee, led the procedure in Scotland. She operated remotely on a human cadaver — a body donated to medical science — using a robotic system capable of replicating the delicate hand movements required in real stroke operations.
A few hours later, neurosurgeon Dr Ricardo Hanel performed the same procedure from Jacksonville, Florida, on another human cadaver in Dundee, successfully conducting a transatlantic robotic thrombectomy more than 4,000 miles (6,400 km) away. The transatlantic connection was powered by high-speed networks and advanced robotics, allowing both surgeons to control fine surgical instruments with astonishing precision and only a 120-millisecond delay, roughly the time it takes to blink an eye.
This dual demonstration has been hailed as a potential game-changer in global stroke treatment. Experts believe the technology could transform access to life-saving care by enabling specialist surgeons to treat patients in real time, even if they are in remote or rural hospitals far from advanced neurovascular centers. Professor Grunwald described the moment as “the first glimpse of the future,” saying that what was once considered science fiction has now become a real and demonstrable possibility.
The University of Dundee, which serves as the global training hub for the World Federation for Interventional Stroke Treatment, played a critical role in this success. It is currently the only place in the United Kingdom where medical professionals can perform interventional procedures on cadavers with synthetic liquid circulating through the vessels, mimicking live blood flow. In this controlled yet realistic environment, the research team was able to carry out every step of a real thrombectomy, proving that the robotic system could replicate human surgical actions with remarkable fidelity.
The experiment used four human cadavers donated to science within the past three years, each embalmed and perfused with a blood-like fluid to simulate living conditions. Both the Dundee and Florida operations used robotic systems developed by the Lithuanian firm Sentante, with advanced imaging and connectivity support provided by technology partners Nvidia and Ericsson.
How the Robotic System Works and Why It Matters
An ischaemic stroke happens when a blood clot blocks an artery that supplies blood to the brain, cutting off oxygen and leading to the rapid death of brain cells. The most effective modern treatment is a mechanical thrombectomy — a delicate procedure in which a specialist threads a catheter through the patient’s blood vessels to physically remove the clot. However, thrombectomy requires highly trained experts and sophisticated equipment that are usually available only in major medical centers.
This presents a serious challenge for patients who live far from such facilities. Stroke outcomes depend heavily on time; as Professor Grunwald emphasized, every six minutes of delay reduces the chance of a good recovery by about 1 percent. For patients in rural or remote areas, that delay can mean the difference between a full recovery and lifelong disability — or even death.
The robotic system demonstrated in Dundee could change this equation entirely. In essence, the technology allows a specialist to perform the operation remotely. A trained medic or nurse at the patient’s local hospital would insert the catheters and connect them to the robotic unit. The specialist, who could be hundreds or even thousands of miles away, would then take control through a remote console. Using fine motor instruments and a real-time visual interface with live X-ray imaging, the remote surgeon can guide wires, capture the clot, and restore blood flow to the brain — all without being physically present.
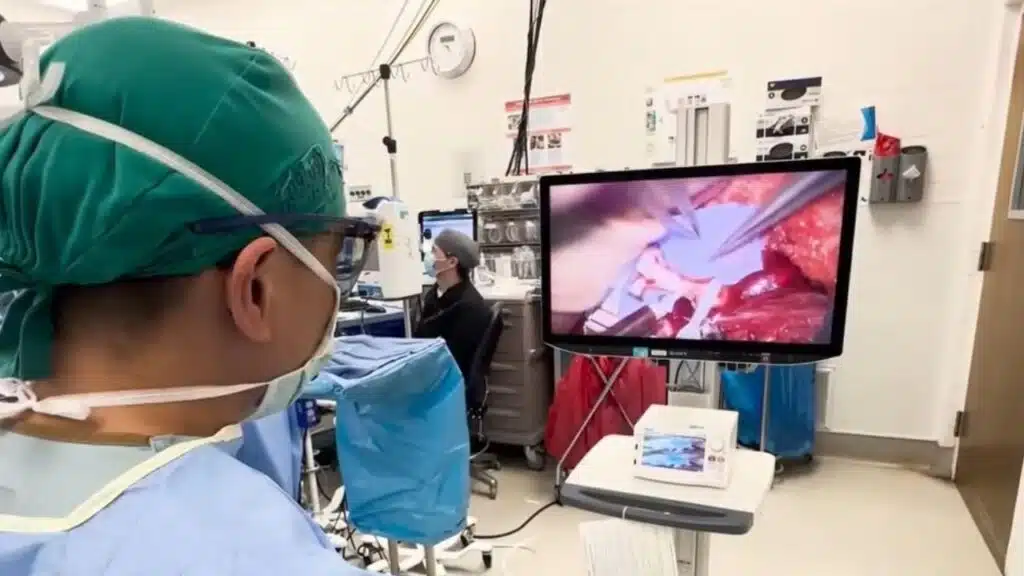
During the trials, both Professor Grunwald and Dr Hanel could view the procedure in real time on screens that displayed live angiographic images of the cadavers’ blood vessels. The robot precisely replicated their hand movements with no perceptible delay, proving that the network connectivity and mechanical responsiveness were sufficient for real-world surgical use. The training time required to operate the system was also remarkably short — less than 20 minutes — suggesting that doctors could adopt the technology quickly once it becomes commercially available and clinically approved.
This innovation directly addresses two of the most pressing problems in stroke care: the shortage of trained specialists and the inequitable access to thrombectomy services. In Scotland alone, only three hospitals — Dundee, Glasgow, and Edinburgh — currently offer the procedure. Last year, there were 9,625 recorded ischaemic strokes in Scotland, but just 212 patients (2.2 percent) received thrombectomy treatment. Across the entire UK, only about 3.9 percent of stroke patients underwent the procedure in the year ending March 2024. These figures highlight a significant treatment gap that robotic intervention could help close by making specialist care geographically independent.
For patients, the potential benefits are immense. Instead of waiting for transfer to a distant hospital, a person suffering a stroke could receive expert treatment at their local facility within minutes. As the robotic system improves, it could also help train new generations of doctors, standardize procedures worldwide, and ensure that high-quality care is available to everyone, regardless of where they live.
Juliet Bouverie, chief executive of the Stroke Association, called the achievement “a remarkable innovation.” She emphasized that patients in rural and remote communities have long been deprived of access to thrombectomy, and that robotic systems like this could finally rebalance the inequality that has persisted in stroke treatment for decades.
Dr Hanel described the experience of operating from across the Atlantic as “truly extraordinary,” noting that it represents not just a technological milestone but a practical step toward saving lives on a global scale. He pointed out that to perform surgery from Florida on a human body in Dundee with a connection lag of only 120 milliseconds was “beyond what we imagined possible.”
The Road Ahead: From Experiment to Real-World Use
While the success of these trials is a historic milestone, the journey toward real-world application is only beginning. The operations were performed on cadavers, not live patients, but the team’s next step is to begin clinical trials on humans within the next year. These studies will test not only the precision and safety of the robotic thrombectomy system but also its reliability in varied medical settings — from urban hospitals to rural clinics connected through high-speed internet.
Professor Grunwald, who recently received an Innovate UK award for her work and serves as the vice-president of the World Federation for Interventional Stroke Treatment, believes the implications extend well beyond stroke care. The same principles could eventually be applied to other time-critical interventions — heart attacks, aneurysms, or trauma surgeries — allowing world-class expertise to be delivered virtually anywhere.
For this vision to become reality, several challenges must be addressed. Regulatory approval will require comprehensive safety data, and hospitals will need robust digital infrastructure with guaranteed low-latency connections. Training protocols, maintenance standards, and cybersecurity safeguards must also be established to ensure the technology is safe from technical failure or digital interference during a live operation.
Still, the optimism among the team is palpable. Edvardas Satkauskas, CEO of Sentante, described the result as proof that “the future is much closer than we think.” His company’s robotic system, combined with cutting-edge imaging and connectivity technology, demonstrates how medical robotics can bridge the gap between geography and expertise.
Public Health Scotland has already expressed strong interest in how such innovations could expand access to advanced stroke care. The success in Dundee and Florida may serve as a blueprint for building an interconnected global network of hospitals, each equipped with robotic units that specialists around the world can operate remotely in emergencies.
Professor Grunwald summed up the vision succinctly: “This technology provides a new way where you are no longer dependent on where you live. It can save those valuable minutes when your brain is otherwise dying.”
If these systems prove safe and effective in live patients, the day may soon come when distance is no longer a barrier to receiving life-saving treatment. The Dundee-Florida collaboration is more than a medical experiment — it is a signal of a new era in remote surgery, one where time, distance, and geography no longer dictate who survives a stroke and who does not.
The Information is Collected from BBC and Yahoo.