A pivotal Phase 1 clinical trial of the experimental CRISPR-based gene therapy CTX310, developed by CRISPR Therapeutics, has demonstrated remarkable efficacy in reducing LDL cholesterol by nearly 50% and triglycerides by about 55% in patients with elevated lipid levels who are resistant to conventional treatments such as statins or other lipid-lowering drugs.
This one-time intravenous infusion targets the ANGPTL3 gene in the liver, permanently silencing it to mimic natural loss-of-function mutations that protect against atherosclerotic cardiovascular disease (ASCVD) without apparent long-term health drawbacks. The results, which exceeded expectations—initial goals were for 30-40% reductions—were presented at the American Heart Association’s Scientific Sessions on November 8, 2025, in New Orleans, and simultaneously published in the New England Journal of Medicine, highlighting the therapy’s potential to shift cardiovascular care from lifelong medications to a single intervention.
Conducted across sites in Australia, New Zealand, and the UK, the trial involved 15 adults aged 31 to 68 with various lipid disorders, including homozygous familial hypercholesterolemia (HoFH), severe hypertriglyceridemia (sHTG), heterozygous familial hypercholesterolemia (HeFH), and mixed dyslipidemias (MDL), all characterized by triglycerides above 300 mg/dL and/or LDL cholesterol above 100 mg/dL (or >70 mg/dL in those with existing ASCVD). This breakthrough builds on CRISPR’s success in rare genetic diseases, extending the technology to more prevalent conditions affecting millions globally, where high cholesterol contributes to the leading causes of death: heart attacks and strokes.
Trial Design and Methodology
The Phase 1 trial was structured as a first-in-human, open-label, dose-escalation study to evaluate the safety, tolerability, and preliminary efficacy of CTX310 in participants with difficult-to-treat hyperlipidemia. Enrollment targeted four cohorts based on lipid profiles: those with HoFH (genetic high LDL), sHTG (extremely high triglycerides), HeFH (milder genetic high LDL), and MDL (combined elevations), ensuring representation across common lipid abnormalities. Doses were administered based on lean body weight, escalating from 0.1 mg/kg (Dose Level 1, DL1) to 0.3 mg/kg (DL2), 0.6 mg/kg (DL3), and 0.8 mg/kg (DL4), with the highest dose given to four patients. Prior to infusion, participants received pre-treatment with corticosteroids and antihistamines to mitigate potential immune reactions, a standard precaution for lipid nanoparticle (LNP)-delivered therapies.
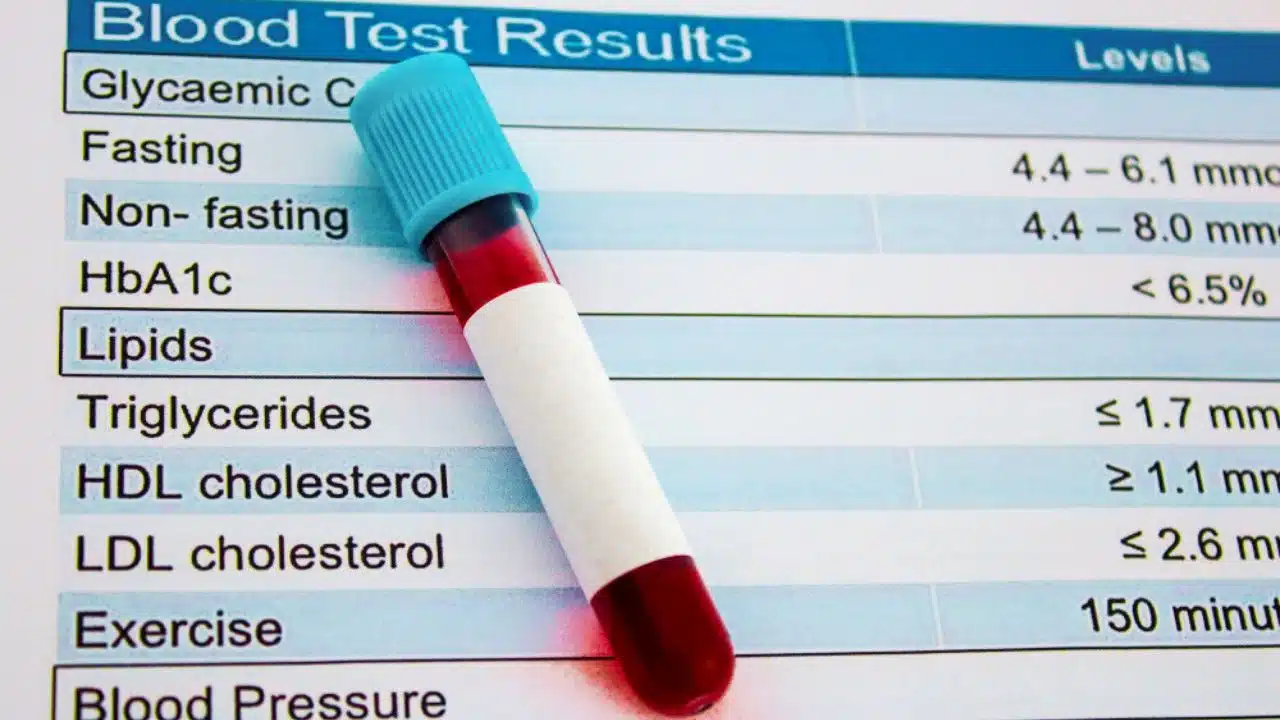
The single infusion lasted up to 4.5 hours, after which patients were monitored for at least 60 days, with ongoing follow-up planned for one year in the trial and up to 15 years for long-term safety as mandated by the FDA for CRISPR-based interventions. Baseline lipid levels were elevated, with median LDL cholesterol at 155 mg/dL and triglycerides at 192 mg/dL, far exceeding recommended thresholds of under 100 mg/dL for LDL in high-risk individuals and under 150 mg/dL for triglycerides.
Efficacy endpoints included reductions in ANGPTL3 protein levels, LDL cholesterol, and triglycerides, measured at multiple timepoints, while safety was assessed through adverse events, liver function tests (e.g., ALT, AST, bilirubin), and complete blood counts. The study’s small size and predominantly male participants limit generalizability, but it provides critical proof-of-concept data for advancing to larger Phase 2 trials with more diverse groups.
Mechanism of Action
CTX310 leverages CRISPR-Cas9 gene-editing technology delivered via lipid nanoparticles to precisely target and inactivate the ANGPTL3 gene in hepatocytes, the primary site of lipid metabolism in the liver. ANGPTL3, or angiopoietin-like protein 3, is a key regulator that inhibits enzymes like lipoprotein lipase (LPL) and endothelial lipase, which normally break down triglycerides and HDL cholesterol while facilitating LDL clearance; by knocking out ANGPTL3, the therapy enhances these processes, leading to sustained reductions in circulating lipids.
The LNP carriers protect the CRISPR components—guide RNA, Cas9 nuclease, and editing machinery—during transit through the bloodstream, enabling them to enter liver cells where the guide RNA directs Cas9 to cleave the ANGPTL3 DNA sequence, creating a double-strand break that disrupts gene expression without repairing to the original form. This approach is inspired by rare genetic variants where ANGPTL3 loss-of-function results in 40-50% lower LDL and triglycerides lifelong, correlating with up to 40% reduced ASCVD risk, as observed in population studies like those from the UK Biobank. Unlike PCSK9-targeted therapies (e.g., earlier CRISPR trials or drugs like evolocumab), which primarily lower LDL, CTX310’s dual action on ANGPTL3 addresses both LDL and triglycerides simultaneously, a significant advantage for patients with mixed dyslipidemias who often require multiple medications.
The editing is durable because it alters the genome permanently, potentially eliminating the need for repeated dosing, though off-target edits are monitored via sequencing to ensure specificity. Animal models prior to human testing confirmed up to 90% ANGPTL3 knockdown with minimal immune activation, paving the way for this translation to clinical use.
Efficacy Results
Preliminary data from the first 10 participants with at least 30 days of follow-up (data cutoff April 16, 2025) showed dose-dependent efficacy, with lower doses (DL1 and DL2) achieving modest ANGPTL3 reductions of around 20-30%, while DL3 and DL4 yielded up to 75% knockdown. At the highest dose (DL4), average LDL cholesterol dropped by 48.9% from baseline within two weeks, stabilizing at similar levels through 60 days, while triglycerides fell by 55.2%, with some patients experiencing even greater benefits.
Compelling individual responses underscore the therapy’s potential: one DL4 patient with sHTG saw triglycerides plummet 82% from 1073 mg/dL to manageable levels by day 30, averting risks like pancreatitis; another DL3 patient with HeFH achieved an 81% LDL reduction from 256 mg/dL by day 90, approaching normal ranges without additional drugs. These outcomes surpassed preclinical predictions, with lipid improvements beginning as early as day 7 post-infusion and persisting without rebound, suggesting stable gene editing.
In the full 15-patient cohort, all doses contributed to meaningful declines, but the highest provided the most robust dual reductions, addressing a gap in treatments for combined hyperlipidemia where current options like fibrates or niacin often underperform or cause side effects. Longer-term data, expected from ongoing monitoring, will clarify if these effects endure beyond 60 days, potentially up to years, mirroring the lifelong benefits seen in natural ANGPTL3 mutants. Overall, CTX310 not only validates ANGPTL3 as a therapeutic target but also demonstrates CRISPR’s precision in vivo for common metabolic disorders.
Safety Profile and Side Effects
Safety was a primary focus, and CTX310 was well-tolerated across all doses, with no treatment-related severe adverse events (SAEs), grade 3 or higher adverse events, or clinically significant changes in liver enzymes (ALT, AST), bilirubin, or platelets observed in a dose-dependent manner. Mild infusion-related reactions occurred in three participants, manifesting as transient back pain, nausea, or chills, which resolved quickly with supportive medications like acetaminophen or anti-nausea agents, and did not lead to discontinuation. One patient experienced a temporary elevation in liver enzymes shortly after screening, which peaked briefly but normalized within days without intervention, attributed possibly to the LNP delivery rather than the editing itself.
No immune-mediated toxicities, such as cytokine release syndrome common in early gene therapies, were reported, thanks to the pre-treatment regimen and the therapy’s liver-specific targeting. One unrelated death occurred months post-treatment due to a pre-existing condition, and the independent data safety monitoring board approved trial continuation. Hematological parameters remained stable, and no evidence of off-target editing or oncogenic risks emerged in initial assessments, though comprehensive genomic analysis continues.
Compared to prior ANGPTL3 inhibitors like evinacumab (which requires monthly infusions and has similar mild side effects), CTX310’s one-time profile appears advantageous, with experts noting its tolerability supports broader application. Long-term surveillance for 15 years will track rare delayed effects, such as liver fibrosis or unintended genetic changes, aligning with regulatory standards for in vivo CRISPR.
Broader Implications for Cardiovascular Health
This trial represents a paradigm shift in managing hyperlipidemia, a condition affecting over 86 million U.S. adults with total cholesterol above 200 mg/dL, by offering a potential “cure” rather than chronic management, which sees 50% non-adherence to statins within a year due to side effects like muscle pain or forgetfulness. For high-risk groups, including those with familial hypercholesterolemia impacting 1 in 250 people or mixed dyslipidemias in diabetics, CTX310 could prevent plaque buildup in arteries, reducing ASCVD events by emulating protective genetics. Cardiologists like Dr. Steven Nissen of Cleveland Clinic described the results as “remarkable,” emphasizing how dual lipid control fills a therapeutic void, potentially lowering heart attack and stroke rates worldwide where cardiovascular disease claims 18 million lives annually.
It also advances equity in care, as underserved populations often face barriers to consistent medication, and a single infusion could be more accessible in resource-limited settings if scaled. Economically, while initial costs may mirror other gene therapies (e.g., $3-4 million for hemophilia treatments), long-term savings from avoided hospitalizations and drugs could justify investment, though pricing details are pending. The American Heart Association’s recent “Lower Your LDL Cholesterol Now” initiative underscores the urgency, revealing that nearly half of survivors don’t know their LDL levels despite high awareness of cholesterol risks. By validating LNP-delivered CRISPR for liver editing, this paves the way for applications in other metabolic diseases like obesity or diabetes.
Future Directions and Challenges
CRISPR Therapeutics plans to present fuller Phase 1 data at a medical conference in the second half of 2025, including extended follow-up beyond 60 days to assess durability, which could extend to years based on the permanent nature of the edit. Phase 2 trials, anticipated soon, will enroll larger, more diverse cohorts—including women, broader age groups, and international participants—to confirm efficacy across ethnicities and validate surrogate endpoints like lipid reductions as predictors of clinical outcomes.
Regulatory pathways with the FDA and EMA will likely accelerate if safety holds, building on CRISPR’s approvals for sickle cell and beta-thalassemia, but challenges remain: optimizing LNP specificity to avoid non-liver uptake, monitoring for rare off-target effects via advanced sequencing, and addressing manufacturing scalability for widespread use. Ethical considerations include equitable access, as gene therapies historically favor wealthier patients, and informed consent for long-term unknowns like secondary cancers, though current data show no such signals. Related programs, like CTX320 targeting another lipid gene, are in parallel trials, suggesting a pipeline of one-time cardiovascular fixes. If successful, CTX310 could debut clinically within 5-7 years, transforming preventive cardiology and reducing the global burden of lipid-driven diseases.