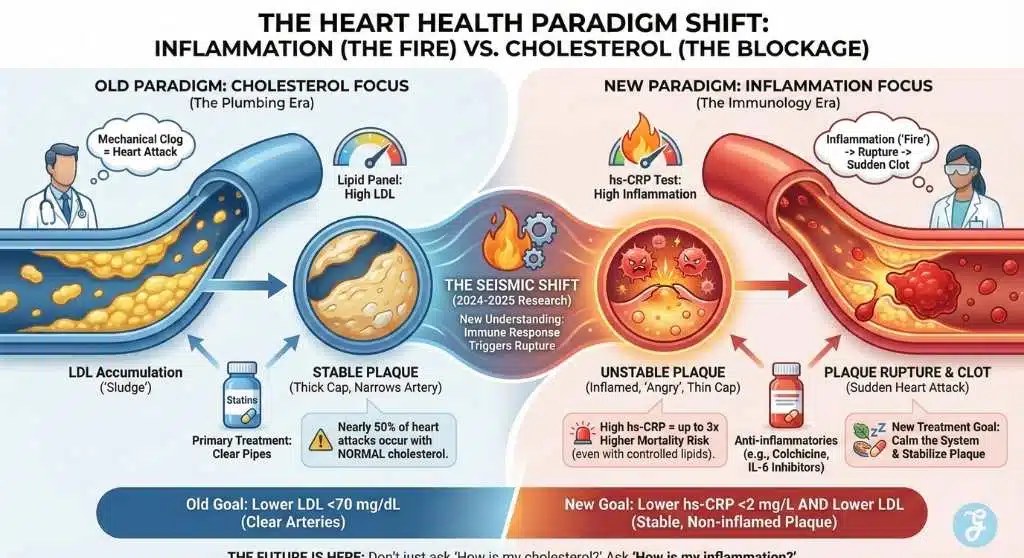
While the world has spent decades fearing cholesterol, a silent killer has been lurking in plain sight: Inflammation. Recent high-profile research, echoed by major medical journals in 2024-2025, has identified C-Reactive Protein (CRP)—specifically high-sensitivity CRP (hs-CRP)—as a predictor of heart disease that, in many cases, outperforms LDL (“bad”) cholesterol. This marks a seismic shift in cardiology and the inflammation vs cholesterol debate. It explains the terrifying phenomenon where fit, healthy-eating individuals with “perfect” lipid panels still suffer sudden, massive heart attacks.
The medical community is now forced to look beyond clogged pipes to the inflamed vessel walls themselves, signaling a new era where treating the “fire” (inflammation) is just as critical as clearing the “blockage” (cholesterol).
Key Takeaways
-
The Paradigm Shift: Heart health is moving from a “plumbing” model (clearing cholesterol blockages) to an “immunology” model (treating vessel inflammation).
-
The Silent Killer: Inflammation (hs-CRP) is a more accurate predictor of heart attacks than cholesterol for many patients, explaining why fit people still suffer events.
-
New Diagnostics: A standard lipid panel is no longer enough. Requesting an hs-CRP test is essential to reveal hidden “residual risk.”
-
Actionable Prevention: Unlike genetic cholesterol, inflammation is highly responsive to lifestyle changes—specifically the Mediterranean diet, weight management, and oral hygiene.
-
Future Treatments: Expect a new wave of targeted therapies, including IL-6 inhibitors and repurposed drugs like Colchicine, to become standard care alongside statins.
Contextual Background: The “Lipid Hypothesis” and Its Limits
For over 50 years, the “Lipid Hypothesis” has dominated heart health. The narrative was simple and mechanical: high saturated fat intake leads to high LDL cholesterol, which accumulates in arteries like sludge in a kitchen drain. This logic birthed the statin era—a multi-billion dollar pharmaceutical triumph that successfully reduced heart attack rates by approximately 25-35%.
But a dangerous gap remained. Nearly 50% of all heart attacks occur in people with normal cholesterol levels. For decades, these cases were treated as bad luck or statistical anomalies. However, the “Inflammation Hypothesis,” championed by pioneers like Dr. Paul Ridker at Brigham and Women’s Hospital, suggested a different mechanism: the body’s immune response to the plaque—not just the plaque’s size—is what triggers ruptures.
Now, in 2025, this hypothesis has graduated to a clinical standard. We have moved from the plumbing era (clearing pipes) to the immunology era (calming the system).
Core Analysis: The Paradigm Shift to Inflammation
The Mechanics
It’s Not Just the Clog, It’s the “Pop”
To understand why inflammation kills, one must understand how a heart attack actually happens. It is rarely caused by a slow buildup that gradually shuts off blood flow. Instead, it is sudden.
- The Stable Plaque: Imagine a hard, calcified bump on the artery wall. It narrows the artery, perhaps causing chest pain during exercise, but it is “stable.” It has a thick cap.
- The Unstable (Inflamed) Plaque: Now imagine a soft, pus-filled boil on the artery wall. It might not block much blood flow, so it passes a stress test. But it is “angry” and inflamed.
- The Rupture: When inflammation markers like CRP are high, immune cells (macrophages) release enzymes that thin the cap of this boil. Under stress, it bursts. The body instantly forms a clot to seal the rupture. This clot is what blocks the artery 100%, causing a heart attack.
The Verdict: You can have a large, stable plaque (high cholesterol) that never ruptures, or a small, inflamed plaque (low cholesterol, high CRP) that kills. The new research confirms that checking the “stability” (inflammation) is as vital as checking the “size” (cholesterol).
The Evidence
The “Residual Risk” Trials
This isn’t just theory; it is backed by landmark trials that changed the guidelines:
- JUPITER Trial: Showed that giving statins to people with normal cholesterol but high CRP reduced heart attacks by nearly 50%.
- CANTOS Trial: A game-changer proving that lowering inflammation without lowering cholesterol (using a drug called canakinumab) significantly reduced cardiovascular events.
- LODOCO2 Trial: Proved that Colchicine, a cheap, ancient anti-inflammatory drug used for gout, drastically reduced heart risks in patients with chronic coronary disease.
The Economic & Industry Pivot
This shift disrupts the pharmaceutical landscape and patient care models, centering on the inflammation vs cholesterol treatment pathways.
- The Statin Plateau: Statin manufacturers face a plateau; their job is “done” for many patients who still have risks.
- The Anti-Inflammatory Gold Rush: We are witnessing a pivot toward “plaque-stabilizing” therapies. New classes of drugs, specifically IL-6 inhibitors (like ziltivekimab) and repurposed drugs like Colchicine, are entering the standard of care.
- Diagnostics Boom: The hs-CRP test ($20–$50) is becoming as mandatory as the lipid panel.
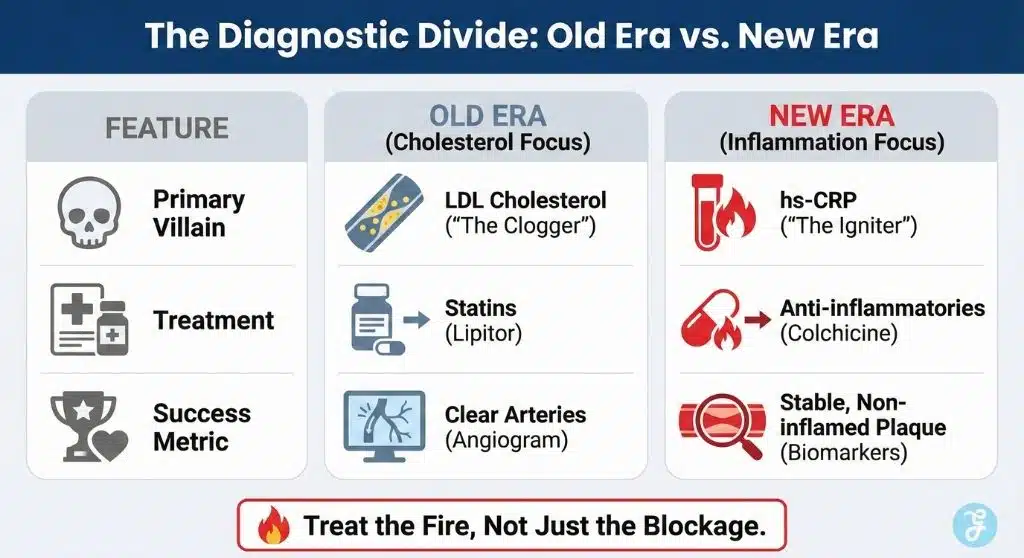
Data & Visualization: The Diagnostic Divide
The following contrasts the traditional view of heart risk with the emerging 2025 standard.
| Feature | The Old Era (Cholesterol Focus) | The New Era (Inflammation Focus) |
| Primary Villain | LDL Cholesterol (“The Clogger”) | hs-CRP (“The Igniter”) |
| Primary Goal | Lower LDL to <70 mg/dL | Lower hs-CRP to <2 mg/L AND Lower LDL |
| Who is at Risk? | People with bad diets, obesity. | Anyone with systemic inflammation (including fit people). |
| Diagnostic Tool | Standard Lipid Panel | Lipid Panel + hs-CRP Test |
| Treatment Focus | Statins (Lipitor, Crestor) | Statins + Anti-inflammatories (Colchicine) + Lifestyle |
| Metric of Success | Clear arteries (Angiogram) | Stable, non-inflamed plaque (Biomarkers) |
Key Statistics (2025 Context)
- 40-50%: Percentage of heart attacks occurring in patients with normal cholesterol.
- 3x Risk: Patients with high CRP are up to 3 times more likely to die from cardiovascular causes than those with low CRP, even if their lipids are controlled.
- Target Level: An hs-CRP level >3 mg/L is now considered “High Risk” (Red Flag). Ideally, you want to be <1 mg/L.
Patient Checklist: When to Request an hs-CRP Test
While universal screening is gaining traction, specific groups should prioritize the inflammation vs cholesterol assessment immediately. You should request an hs-CRP test if:
- You have “normal” cholesterol but a family history of heart disease.
- You have an autoimmune condition (Rheumatoid Arthritis, Lupus, Psoriasis), as these systemic inflammatory diseases double heart risk.
- You have metabolic syndrome, even without full-blown diabetes (belly fat, borderline high blood pressure).
- You have a history of gum disease (periodontitis), a proven source of vascular inflammation.
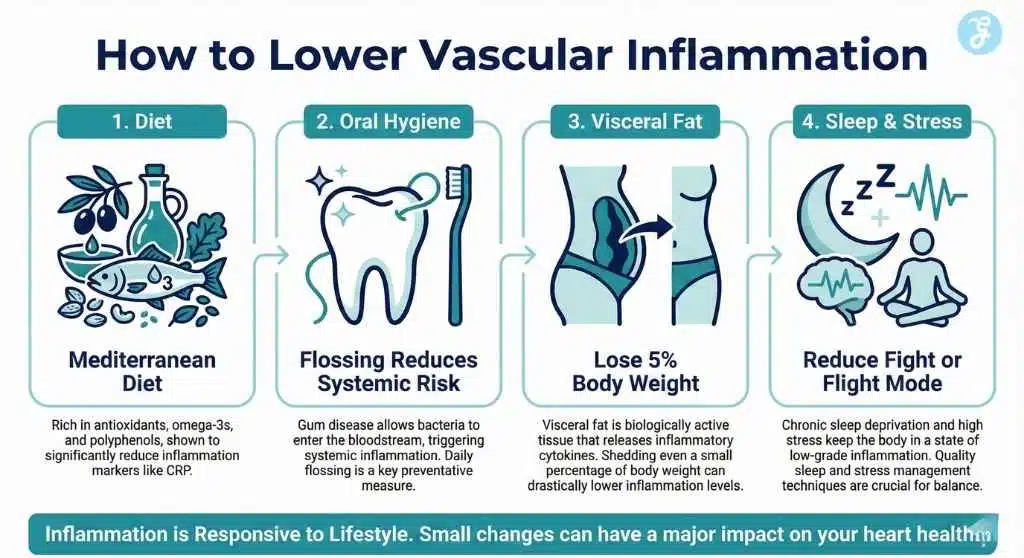
Actionable Insights: How to Lower CRP (Beyond Drugs)
While cholesterol is heavily genetic (influenced by Lp(a)), inflammation is highly responsive to lifestyle. This empowers the patient.
- The “Inflammatory Diet”: Sugar and processed flour are the biggest triggers. They cause insulin spikes, which trigger the liver to produce CRP. The Mediterranean Diet (rich in olive oil, nuts, and fatty fish) is the gold standard for lowering CRP.
- Oral Hygiene: There is a direct link between gum disease (periodontitis) and heart attacks. Bacteria from infected gums enter the bloodstream, raising systemic CRP. Flossing is effective heart protection.
- Visceral Fat: Belly fat is not just storage; it is active tissue that pumps out inflammatory cytokines (IL-6). Losing even 5% of body weight can drastically drop CRP.
- Sleep & Stress: Chronic sleep deprivation keeps the body in a “fight or flight” mode, maintaining low-grade inflammation.
The Risks: Balancing Immunity and Heart Health
The shift to treating inflammation is not without peril. Unlike lowering cholesterol, which has few downsides, lowering inflammation impacts the immune system. Aggressive anti-inflammatory therapies (like Canakinumab or high-dose steroids) can leave patients vulnerable to fatal infections (sepsis).
This is why the “Inflammation vs Cholesterol” era requires precision. The goal is to lower vascular inflammation without shutting down the body’s ability to fight off the flu or pneumonia. This delicate balance is currently the biggest challenge for cardiologists prescribing new therapies like Colchicine.
Future Outlook: What Comes Next?
The Rise of “Inflammation Typing”: By 2026/2027, “heart disease” will likely cease to be a single diagnosis. Just as cancer has subtypes, we will see cardiac patients typed by their driver:
- Type A: Cholesterol-driven (Needs PCSK9 inhibitors/Statins).
- Type B: Inflammation-driven (Needs IL-6 inhibitors/Colchicine).
- Type C: Mixed.
The Ziltivekimab Era: Watch for the approval and rollout of ziltivekimab. Unlike general anti-inflammatories that might lower immunity (raising infection risk), this drug specifically targets the IL-6 pathway related to atherosclerosis, promising a “sniper” approach to heart inflammation rather than a “shotgun.”
Personalized Wearables: Current wearables track heart rate. Future devices (continuous biochemical monitors) will likely track inflammatory markers in sweat or interstitial fluid, alerting users to “inflammatory spikes” caused by stress or poor diet in real-time.
Closing Thoughts: The Future of Heart Health
The identification of CRP as a “villain” equal to or greater than cholesterol is not just a medical update; it is a rewrite of the rulebook. It validates the experiences of millions who did “everything right” yet suffered heart events.
As we move forward, the focus shifts from merely unclogging the pipes to cooling the system down. For the patient, the message is clear: Don’t just ask your doctor, “How is my cholesterol?” Ask, “How is my inflammation?”