The first human prime editing data have been published in the New England Journal of Medicine, describing early results from a Phase 1/2 trial of Prime Medicine’s investigational therapy PM359 in two people with a rare immune disorder called p47-phox chronic granulomatous disease (CGD).
The peer‑reviewed report marks the first time clinical outcomes from a prime editing treatment have appeared in a major medical journal, moving the technology from theory and preclinical work into documented human evidence.
What has just been published?
Prime Medicine announced that NEJM has published a clinical report describing initial results from two patients treated with PM359, a prime‑editing–based therapy designed for p47-phox CGD, an inherited immune deficiency that leaves patients highly vulnerable to severe infections. The article presents first‑in‑human data on safety, biological activity and early signs of efficacy, based on a multinational Phase 1/2 study that aims to follow both adult and pediatric participants over time.
According to company statements summarizing the NEJM paper, both reported patients showed rapid recovery of blood cell production (engraftment) after receiving their edited stem cells, together with restoration of the cellular enzyme activity that is defective in CGD. No major safety signals clearly linked to the prime editing intervention were reported in these early follow‑up data, though longer observation and more participants will be needed to fully define the risk profile.
How prime editing works and why this trial matters
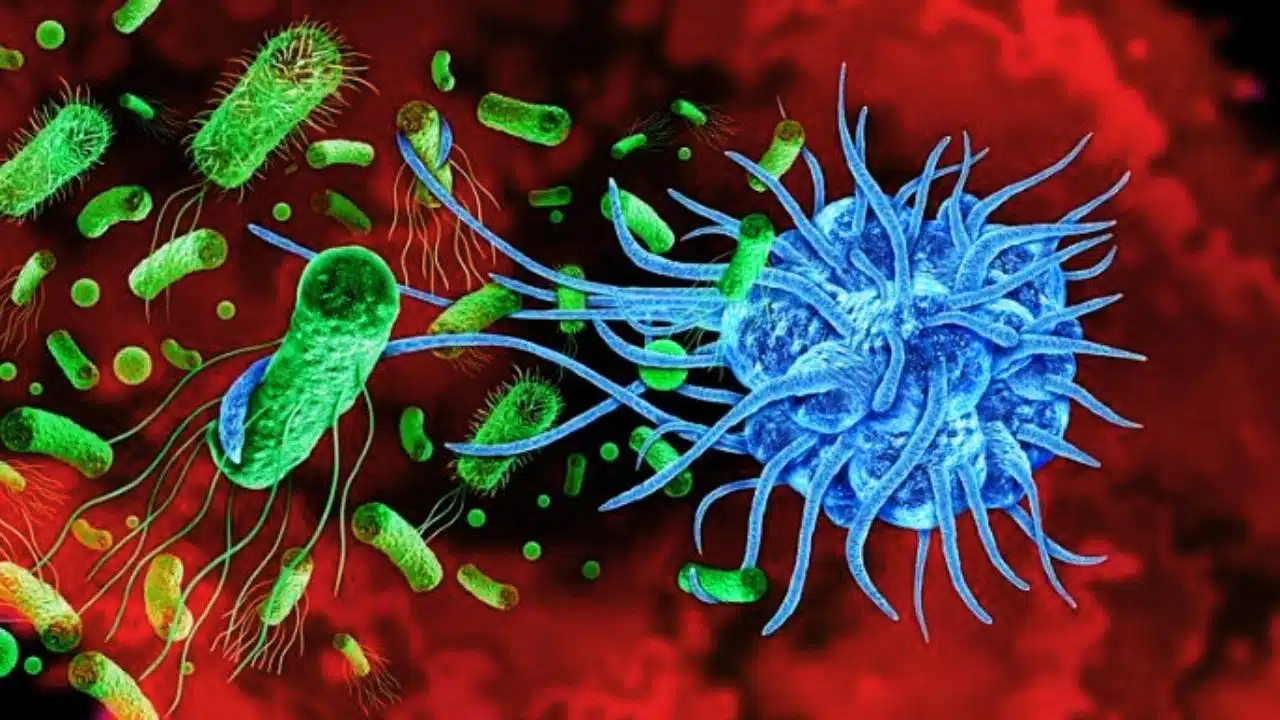
Prime editing is a newer member of the CRISPR gene editing family that uses a modified Cas9 enzyme fused to a reverse transcriptase to rewrite DNA letters without cutting both strands of the genome. Unlike traditional CRISPR approaches that create double‑strand breaks and rely on the cell’s repair machinery, prime editing aims to directly install precise genetic changes, including all possible base substitutions and small insertions or deletions, with fewer unwanted edits.
The technique was first described in 2019 by a team led by David Liu and has since been tested extensively in cells and animal models, but until recently remained largely preclinical. Earlier in 2025, Nature reported that prime editing had been used for the first time to treat a teenager with a rare immune disorder, highlighting the technology’s debut in the clinic. The new NEJM publication adds peer‑reviewed clinical evidence, providing physicians, regulators and researchers with detailed data rather than only company presentations or conference updates.
Prime editing milestone timeline
| Year | Milestone (paraphrased) | Source |
| 2019 | Prime editing method first described as a versatile, precise gene‑editing platform. | Academic review on prime editing |
| 2023 | Experts predict first clinical prime editing trial will begin around 2024. | Gene therapy commentary |
| 2024 | US FDA clears an IND for PM359, the first prime editing therapy to enter human trials for CGD. | Regulatory and industry reports |
| 2025 (mid‑year) | Initial clinical update: first‑ever human clinical data show safety and activity of prime editing in a CGD patient. | Specialist CRISPR and rare‑disease news |
| 2025 (Dec.) | NEJM publishes first detailed human prime editing data for two PM359‑treated patients with p47-phox CGD. | Company announcement and financial news summaries |
Inside the PM359 trial and early results
PM359 targets a specific mutation in the NCF1 gene, which encodes the p47-phox component of the NADPH oxidase complex; defects in this complex cause one common form of CGD by preventing immune cells from generating microbe‑killing reactive oxygen species. In the Phase 1/2 study, patients’ blood‑forming stem cells are collected, edited ex vivo with the prime editing system to correct the NCF1 mutation, and then reinfused after myeloablative conditioning, a standard preparative regimen used in stem‑cell transplants.
Company summaries of the NEJM paper state that both reported patients experienced rapid engraftment of neutrophils by around two weeks after transplantation and platelet recovery shortly thereafter, faster than median recovery times reported for some existing gene‑editing approaches. Functional testing showed restoration of NADPH oxidase activity in neutrophils, and clinically, patients began to show improvement in infection‑related symptoms, consistent with a recovering immune system.
Key data from the first NEJM report (as disclosed)
| Feature | Reported detail (paraphrased) | Source |
| Condition | p47-phox chronic granulomatous disease, a rare inherited immune deficiency. | Clinical and company reports |
| Therapy | PM359, an ex vivo prime‑editing therapy targeting an NCF1 mutation in stem cells. | Trial descriptions |
| Trial phase | Ongoing Phase 1/2 first‑in‑human, multinational study. | Regulatory and company material |
| Patients in NEJM report | Two individuals (adult and pediatric) with severe CGD manifestations. | Publication summaries |
| Engraftment | Rapid neutrophil and platelet engraftment roughly within the first three weeks after infusion. | Clinical updates |
| Biological activity | Restoration of NADPH oxidase function in neutrophils in both patients. | Company and specialist coverage |
| Safety (early) | No prime‑editing–related serious safety concerns reported in initial follow‑up; monitoring continues. | Company and news reports |
Because only two patients are described and follow‑up is still relatively short, experts emphasize that the findings should be viewed as proof‑of‑concept rather than definitive evidence of long‑term benefit or safety. Regulators will likely require data from a larger cohort and longer monitoring to look for delayed complications such as clonal blood cell expansion or off‑target edits, issues that have been central to the evaluation of other gene‑editing therapies.
What this means for gene therapy and what comes next
The NEJM publication places prime editing alongside established gene‑editing platforms such as CRISPR‑Cas9 and base editing, which have already produced approved therapies for conditions like sickle cell disease and transfusion‑dependent beta thalassemia. Analysts note that, if the encouraging PM359 trends hold up in more patients, prime editing could offer a way to correct a wide variety of pathogenic mutations with potentially fewer off‑target effects and less genomic disruption than technologies that rely on double‑strand DNA breaks.
Prime Medicine has indicated that it plans to continue enrolling patients and expanding follow‑up, while also advancing additional prime‑editing programs for other genetic diseases if the safety and efficacy profile remains favorable. Beyond this single trial, academic and industry groups are already exploring prime editing for blood disorders, metabolic diseases and other inherited conditions, but most of those efforts remain preclinical or at very early clinical stages. For patients and clinicians, the key questions now are how durable the edits prove to be, whether unexpected safety issues emerge over years rather than months, and how quickly such complex, individualized treatments can be scaled and made accessible if they succeed.