Medical billing is a strenuous task. Denials of healthcare claims are a chronic issue for healthcare providers. A small error can lead to denied claims and a huge loss of money and time. As reported by Experian Health in the ‘State of Claims 2024’ report, 65% of respondents believe that it is harder to submit “clean” claims now than it was before the pandemic. Moreover, 46% of the respondents mention missing or incorrect data as one of the leading reasons for denials.
Medical billing claim scrubbing is the optimal method to review claims for errors prior to submitting them to payers. Claim scrubbing is a third-party-provided service to medical providers. Its major function is to identify and remove errors in billing codes, minimizing
the number of rejected or denied claims. It is a method of auditing claims before presenting them to insurers. The following sections discuss the claim scrubbing process and its advantages in medical billing.
What is Claim Scrubbing in Medical Billing?
Claim Scrubbing is the process of identifying and eliminating coding issues from medical claims prior to presenting them to insurers. Claim scrubbers, check your claims for Current Procedural Terminology (CPT) codes. An incomplete error in the relevant five-digit code (whether brought about by computer programs or human errors) could lead to a claim denial.
Third-party medical billing companies provide claim scrubbing via software or clearinghouse enrolments. A claim scrubbing software, using automated rule engines, searches for errors that can cause a claim rejection.
It is a comprehensive quality control process that ensures that claims meet regulatory requirements, medical coding rules, and payer standards.
Advantages of Scrubbing Claims
Scrubbing claims is a crucial process in the medical billing procedure. It transforms and enhances your revenue cycle by lowering the rate of denied claims. Claim scrubbing assists with immediate refunds and improves cash flow. Additionally, some of the advantages of cleaning claims are as follows:
Flawless Claims Submission
Claim scrubbing significantly reduces the risk of claim denials by finding and correcting any potential errors and discrepancies in claims prior to submission. It minimizes the administrative burden of appealing denied claims and ensures a stable income stream.
The process will ultimately simplify payment collection on your part and enhance the accuracy of insurance claim submissions.
As a result, you will have fewer and fewer problems getting timely and complete insurance company payments.
Fewer Claim Rejections
A doctor has to submit a claim to receive payment after administering medical treatments and healthcare services. But submitting claims can be a challenging and complicated process, and there is a high rate of errors. When you scrub a claim, it identifies and corrects errors prior to claim submission.
Claims scrubbing reduces the likelihood of denials by finding and correcting errors. It helps in ensuring that claims are thorough, accurate, and comply with the specific billing specifications of insurance payers. Consequently, there are cleaner claims, which increases the likelihood of timely and accurate compensation.
Improved Revenue Cycle
A claim scrubbing process increases the likelihood of accurate and clean claim submissions. It accelerates the payment cycle by minimizing errors and streamlining the claim submission process. Claim scrubbers improve billing accuracy and ensure your claims are accepted on the first attempt. When a third party scrubs a claim of any healthcare provider, it enhances operational efficiency and financial stability.
Insurance companies, therefore, provide timely payments for medical treatments. You can also use the improved revenue collection from the claims cleansing process to fund your clinic’s operations.
Quality Patient Care
Rejected claims challenge the patient-provider relationship and upset the payers. When a claim is denied, the patient and provider lose valuable time and money. An effective claims-scrubbing solution will ensure the best possible experience for all parties while saving these valuable resources.
Scrubbing your claims ensures that each claim is correct and timely, which results in satisfied patients who are more inclined to trust you in the years to come.
Manually scanning your claims takes time and is prone to human error. An automated claim scrubber speeds up the process and its effectiveness. As a result, staff and doctors have more time to engage with and care for patients.
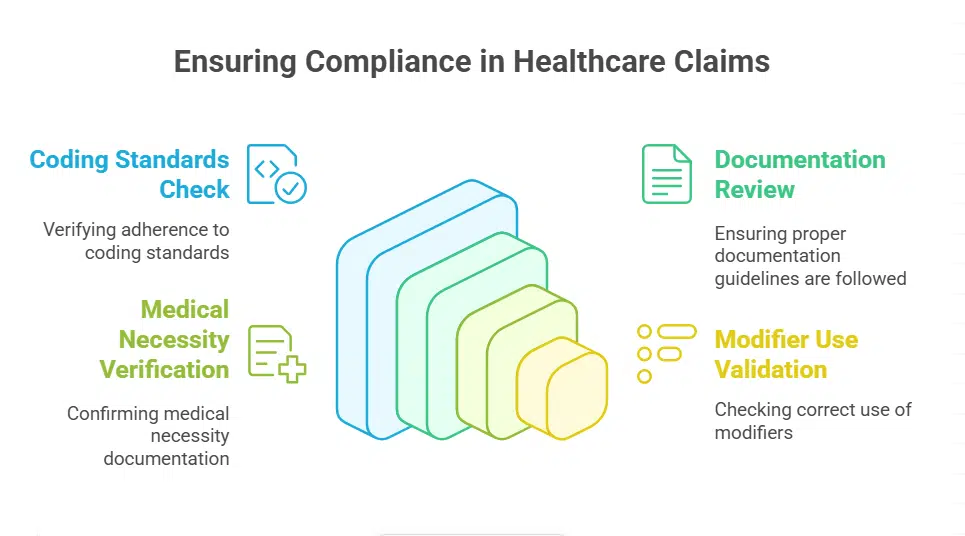
Regulatory Compliance
Claims scrubbing can help healthcare organizations maintain compliance with several payer obligations and regulations. This ensures that coding standards, documentation guidelines, and other important requirements are followed, which reduces the likelihood of audits, penalties, and legal issues.
When filing claims, one must adhere to the regulations and instructions set out by various insurance payers. Claim scrubbing in medical billing guarantees that the claims follow these guidelines, averting possible non-compliance problems. It entails verifying that medical necessity paperwork, modifier use, and coding are all done correctly.
Challenges in Medical Claims Scrubbing
Medical billing claim scrubbing is difficult but essential for healthcare facilities. By resolving the following three challenges in claim scrubbing, medical providers can ensure more streamlined operations and a more predictable revenue flow.
Delayed Claim Submission
While claims scrubbing in medical billing introduces an additional level of review, it also pushes claim submission later since every claim has to be scrubbed/reviewed first before being sent to the insurance payer. When claims are submitted after the filing deadline, the insurance payers reject them, and even the appeals process runs longer than required. You need to develop accurate procedures and processes for the timely filing of data and claims to prevent such hassle. Ensure that all information that is pertinent information is collected and verified while the patient is on a visit.
Not Verifying Patient Eligibility
Keeping pace with continually changing rules, code updates, and payers’ requirements might be difficult, particularly when failure to comply might result in financial losses. Being compliant with the Health Insurance Portability and Accountability Act (HIPAA) regulations is essential for protecting the confidentiality of patients and preventing costly fines and legal issues.
Implement a standard procedure for checking the patient’s eligibility, benefits, and coverage information, and invest in claims scrubbing after putting strong security measures in place for encrypting data. Develop a compliance team or appoint a compliance officer to watch and advise about rule changes.
Shortage of Staff
Claim scrubbing in medical billing requires a specialized understanding of coding, compliance, and insurance standards. However, many healthcare practitioners, particularly those in smaller or rural practices, need help to offer the required training or deal with a lack of trained workers.
Invest in staff training to educate them on the most recent coding standards and payer regulations. Employees with proper training can spot mistakes and fix problems throughout the claim scrubbing procedure.
Claims Scrubbing Process
The claim scrubbing process includes more than twenty stages to authorize payments against the rendered care services.
To keep the process simple, let’s examine what occurs following a patient encounter:
- The billing department should submit a claim within 48 hours of service.
- They conduct an algorithmic first review to prevent mistakes, inaccuracies, or duplicate charges.
- Next, they determine eligibility by checking the database to identify if the patient has an active insurance plan under his name and policy number.
- The location of the medical facility and the information about the healthcare practitioner are checked to ensure they are included in the network.
- The algorithm applies established costs after reviewing the services the doctor has billed for.
- The patient’s benefits are assessed for the services rendered via the system.
- The system checks the claim to ensure the billed services and/or items are safe for the patient, compliant with industry best practices, and medically necessary.
- A risk assessment is performed to see if a claim is low-risk or high-risk for insurance fraud based on the services rendered, expenses, and total costs on the bill.
- The doctor receives the appropriate compensation for the services based on pre-determined prices.
- The insurance firm explains benefits to show how and what the doctor was paid and how much the patient would have to pay out of pocket.
- The amount and services listed in the doctor’s explanation of benefits should match the bill the patient receives.
Bottom Line
In the always-changing healthcare landscape, it is impossible to overestimate the significance of claim scrubbing.
If you find it difficult to scrub a claim or lack the necessary expertise, consider partnering with one of the leading healthcare RCM companies. It can minimize your hassles and help you improve the efficiency of your claim-processing workflow.