Are you dealing with sharp and sudden pain in your rectum or anus? Proctalgia fugax is a functional anorectal disorder that causes intermittent episodes of rectal pain. In this article, we’ll explain the symptoms, causes, diagnosis, and treatment options for proctalgia fugax so you can experience relief from these debilitating moments.
Plus, stay updated on any emerging research related to effective treatments for this condition. Get ready to learn all about proctalgia fugax – let’s jump right in!
Content Highlights
- Proctalgia fugax is a functional anorectal disorder characterized by recurrent and fleeting episodes of intense rectal pain.
- Common triggers for proctalgia fugax include physical activities such as exercise or straining during bowel movements, stress, constipation, and dietary changes.
- The diagnosis typically involves medical history taking coupled with physical examination and, in certain cases, additional tests like X-rays or MRI to identify underlying medical conditions.
- Treatment options may include self-care measures such as pelvic stretching/breathing, medications, relaxation techniques, and physical therapy to ease the pain associated with proctalgia fugax.
What Is Proctalgia Fugax?
Proctalgia fugax is a type of anorectal disorder characterized by recurrent and fleeting episodes of intense rectal pain.
Definition and explanation
Proctalgia fugax is an intermittent, recurring, and self-limiting pain in the anorectal region. It differs from chronic proctalgia which is a separate condition characterized by a dull ache or pressure sensation high up in the rectum.
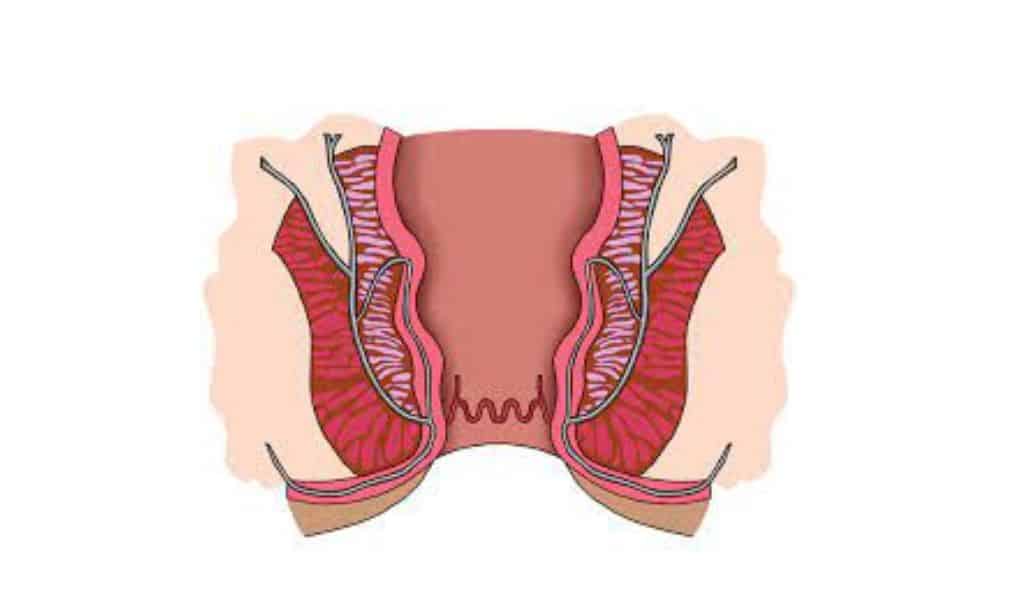
The cause of proctalgia fugax remains unclear, but it is believed to be linked to muscle spasms inside or near the anal sphincter. Symptoms include brief episodes of severe rectal pain that can even wake a person up during sleep, with no symptoms occurring in between episodes.
Treatment options for proctalgia fugax are not plenty, but some individuals have reportedly found relief through warm baths, anal relaxation exercises, or muscle relaxant medications.
Symptoms and duration
Proctalgia fugax is characterized by sudden and intense episodes of rectal pain. The pain is typically described as sharp, stabbing, or cramp-like in nature. Each episode usually lasts between a few seconds to around 30 minutes, although this can vary from person to person.
Generally speaking, no underlying medical condition underlies proctalgia fugax, and it rarely leads to any serious complications. It has been observed that episodes of severe rectal pain can be triggered by stressful events, physical activities such as exercise or straining during bowel movements or sexual intercourse, constipation, and/or dietary changes.
Thus managing stress levels may help reduce the severity and duration of these painful episodes over time.
Proctalgia Fugax vs. Levator Syndrome
Despite some similarities, Proctalgia Fugax is distinct from Levator Syndrome in terms of symptoms, etiology, and treatment.
Differences and similarities
Between Proctalgia Fugax and Levator Syndrome similarities include being types of anal pain and having physical and emotional triggers. However, their symptoms, duration, and methods of management differentiate them.
| Proctalgia Fugax | Levator Syndrome | |
|---|---|---|
| Type of Disorder | Functional anorectal pain disorder | Pelvic floor dysfunction |
| Characteristics of Pain | Intermittent, recurring, and self-limiting pain | Chronic, vague, dull ache or sensation |
| Duration of Pain | Typically lasts less than 20 minutes | It can last several hours |
| Symptoms Between Episodes | No symptoms in between episodes | Symptoms can persist even in between episodes |
| Triggers | Many triggers, including physical and emotional factors | Often triggered by sitting for long periods or stress |
| Management | It can be managed through self-care measures, medications, relaxation techniques, and physical therapy | Often treated with physical therapy, biofeedback, and pain relief medications |
Table: Differences Between Proctalgia Fugax and Levator Syndrome
Causes and Triggers of Proctalgia Fugax
Physical, Emotional, and Dietary factors may be the source of rectal pain associated with Proctalgia Fugax. Dive in deeper to explore what triggers this condition.
Physical factors
- Sexual activity: Engaging in sexual activity can sometimes cause proctalgia fugax due to increased muscular tension and spasms of the anal area.
- Stress: Mental or emotional stress can often put extra strain on the muscles in the rectal area, which can trigger episodes of pain associated with this condition.
- Constipation: Difficulty with defecation due to hard stool or other bowel issues such as irritable bowel syndrome (IBS) may cause extra pressure on the muscles around your anus, leading to a proctalgia episode.
- Defecation: The act of passing stools itself may be a factor that triggers an episode, as straining and pushing during defecation may lead to muscle spasms and pain in some individuals suffering from proctalgia fugax
Emotional factors
- High anxiety or stress can be triggers for episodes of proctalgia fugax.
- Anxiety and panic disorders have been linked to flare-ups of rectal pain from the condition.
- Intense emotional distress has also been associated with instances of anal discomfort in people with the disorder.
- An association between depressive symptoms and an increased risk for proctalgia fugax has been suggested in recent research.
Dietary factors
- Dietary factors can contribute to proctalgia fugax, and it is important to maintain a high-fiber diet with plenty of fruits and vegetables.
- Eating fiber-rich foods such as whole grains, nuts, legumes, and oats helps keep the digestive system healthy.
- Foods like apples, bran cereals, and flaxseeds are packed with dietary fiber that helps prevent constipation which may be related to anal discomfort.
- Fruits and vegetables should make up a large portion of one’s diet in order to get adequate fiber intake. Essential vitamins are also found in these natural sources, which help balance digestion.
- Drinking enough water each day is essential for proper hydration and regular bowel movements. Alcoholic beverages can have a dehydrating effect on the body, so it’s best avoided if possible.
Caffeine should also be reduced or eliminated from the diet as its stimulating effect can cause gastrointestinal distress when consumed in excess amounts.
Diagnosis of Proctalgia Fugax
Diagnosis typically includes a medical history, physical examination, and in some cases, additional tests such as X-rays or MRI.
Medical history
A patient’s medical history plays an integral role in diagnosing proctalgia fugax and ruling out other potential causes of anorectal pain. Doctors and healthcare professionals will use the information gathered from a patient’s medical history, such as their age, gender, lifestyle factors, family health conditions, and other chronic or acute illnesses, to help narrow down potential diagnoses.
The doctor may also ask questions about any medications that are being taken or lifestyle habits, such as smoking which can contribute to this condition. Combining the assessments made during the physical examination with those from the taking of a detailed medical history provides doctors with invaluable insight into accurately pinpointing a diagnosis for their patient’s anorectal pains.
In addition to these assessment techniques, additional diagnostic tests may be utilized if certain red flags arise within the context of medical history taking itself. Tests such as x-ray imaging or lab work might provide further proof that will allow physicians to confidently diagnose proctalgia fugax in patients who suffer from similar symptoms stemming from various underlying causes.
Ultimately, gathering all pertinent information contained within each individual’s medical history gives clarity when working towards diagnosing procoltalia fugax so that the most suitable treatment options can be implemented for the successful management of symptoms.
Physical examination
Physical examination is an essential step in the diagnosis of proctalgia fugax. During the physical exam, the healthcare provider will examine your abdomen and rectum to assess for abnormalities or underlying medical conditions that may be causing the pain.
They may also include a digital rectal exam (DRE) whereby they insert a gloved finger into your rectum to further check for any issues, such as blockage or tenderness in certain areas.
Other tests, such as urine analysis, blood workup, CT scans, etc., might be recommended if other possible causes are suspected. A physical examination helps rule out any serious medical conditions at play and can provide helpful clues regarding what’s causing proctalgia fugax symptoms.
Other diagnostic tests
Diagnosing proctalgia fugax can be challenging due to the random and quick nature of the spasms. While there are no specific diagnostic tests for this condition, some general diagnostic steps may be taken, including:
- Medical history – The patient’s reported symptoms, as well as any medical and family history, should be recorded.
- Physical examination – A physical exam may help rule out other potential causes of anorectal pain, such as hemorrhoids or anal fissures.
- Lab & imaging tests – Various lab tests such as blood work along with a rectal ultrasound, X-ray scan, magnetic resonance imaging (MRI), or computerized tomography (CT) scans may used to diagnose digestive disorders, which could contribute to proctalgia fugax-related pain.
- Psychological assessment – A psychological assessment may also take place to evaluate if any mental health conditions are causing stress which could trigger episodes of anal spasms in some cases.
Treatment Options for Proctalgia Fugax
Various treatment options, such as self-care measures, medications, relaxation techniques, and physical therapy, can be employed to help ease the pain associated with proctalgia fugax.
Self-care measures
- Pelvic stretching: It involves lying on your back with both legs bent and feet flat on the floor. Then, take a deep breath in, and as you exhale, slowly pull one of your legs up towards your chest for 10 seconds or so while relaxing the other leg. Make this motion two to three times per side every day until it becomes easier and more comfortable for you to perform.
- Pelvic breathing: Just like abdominal breathing, pelvic breathing focuses on controlling the flow of air by using different sets of muscles around the abdomen area – specifically those that control contraction and relaxation of the pelvis region. To do it correctly, sit comfortably with your spine straight but relaxed, then inhale deeply, focusing all attention on filling out all corners surrounding the old belly button (360 degrees). Slowly tilt your pelvis forward until a gentle stretch is felt at lower back/abdomen areas; hold for 3-5 seconds; then release aggressively, pushing away air from lungs in multiple directions – up through chest right into book twist (.e rotation left) then down through abs finishing at vertical line passing between hip bones – thereby completing movement circle powered by slow controlled breaths
- Sitz bath: A sitz bath includes sitting in warm water about knee height or less to help reduce swelling, pain, irritation, or itching associated with proctalgia fugax symptoms. The use of essential oils such as lavender can be added to these baths as well. Generally speaking, they should be done once a day just before bedtime
- Topical medication: If experiencing intense throbbing pain from proctalgia fugax episodes applying topical medications like lidocaine cream may relieve symptom intensity.
Medications
Simple analgesics and nonsteroidal anti-inflammatory agents are the first forms of treatment for proctalgia fugax. These medications work by blocking certain hormones that cause inflammation, resulting in reduced pain.
Relaxation techniques
- Meditation: Focus on your breathing and observe any physical or mental sensations that may arise.
- Deep-breathing exercises: Inhale deeply for 3 seconds, hold the breath for 4 seconds, then exhale slowly for 5 seconds with a slight pursed lip motion to reduce tension in the diaphragm and abdomen.
- Yoga poses: Gentle stretching yoga poses like cobra, bow pose, and cat/cow flow can help relax tight muscles that are associated with proctalgia fugax spasms.
- Warm baths or sitz baths: Spending 10-15 minutes in warm water promotes relaxation of the anal sphincter muscle, easing discomfort associated with proctalgia fugax attacks.
- Progressive Muscle Relaxation (PMR): Alternately tightening and releasing different groups of muscles throughout the body helps to release tension held deep within physiological cells, which helps when suffering from persistent episodes of haunting pain.
Physical therapy
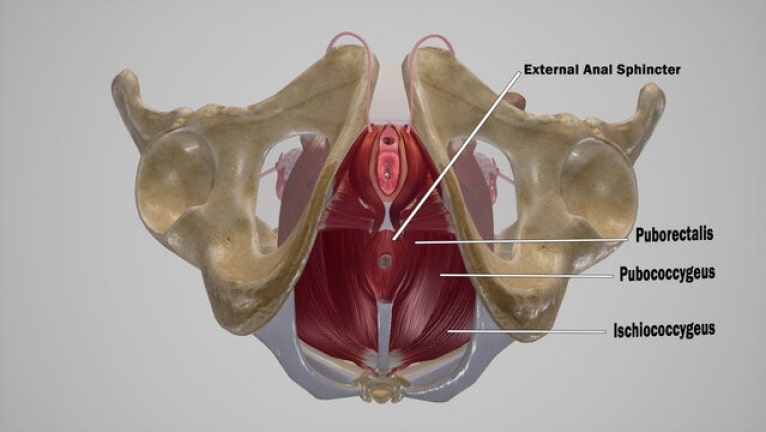
Physical therapy can be an effective treatment option for managing proctalgia fugax. Physical therapists are able to assess and evaluate muscle tension, spasms, and other bodily issues associated with the condition in order to develop targeted therapeutic exercises that help relieve symptoms.
Techniques such as muscle stretching, abdominal strengthening, pelvic floor relaxation exercises, biofeedback training, nerve flossing techniques, and heat therapy can all be used by physical therapists when treating proctalgia fugax.
These types of non-invasive treatments not only improve muscular relaxation but can also reduce stress levels which further helps alleviate pain caused by the condition. With a personalized plan of physical therapy tailored to each patient’s individual needs, many individuals find that these forms of treatments help them significantly manage their proctalgia condition without having to resort to medication or more invasive treatments.
Managing Stress and Proctalgia Fugax
Knowing how to manage stress is important for the effective treatment of proctalgia fugax, as managing chronic tensions in your muscles can help reduce the frequency and intensity of rectal spasms.
Stress reduction techniques
- Deep breathing: Taking deep breaths is a simple but effective technique for relieving stress. With each inhale, focus on filling your lungs and abdomen, then exhale slowly to complete the cycle.
- Mindfulness practices: Practicing mindfulness can help shift your attention away from feelings of stress or anxiety towards being fully aware of the present moment.
- Relaxation techniques: Techniques such as progressive muscle relaxation can be used to bring awareness and release tension in various parts of the body and ultimately lead to improved relaxation.
- Cognitive-behavioral therapy (CBT): CBT helps to identify distorted patterns of thinking that contribute to increased levels of stress while working with patients through therapeutic conversations and exercises designed to develop healthy coping skills for managing their condition more effectively.
- Stress management strategies: Developing personalized plans that include lifestyle changes such as physical activity routines, healthy diet habits, and adequate restful sleep will benefit individuals who suffer from proctalgia fugax by reducing symptoms associated with chronic pain or anxiety resulting from disrupted life balance.
Therapy and counseling
Therapy and counseling may be recommended as part of treatment for proctalgia fugax when it is emotionally or psychologically related. Counseling can help individuals develop strategies to cope with stress, anxiety, depression, and other mental health issues associated with the condition.
It may also provide them an outlet to discuss their struggles and gain insight into behavior patterns contributing to their symptoms. Therapy sessions might involve cognitive-behavioral therapy (CBT) or psychotherapy, which focuses on reducing overall psychological distress while utilizing relaxation techniques.
Developing healthy coping strategies through therapy can ultimately lead to better emotional well-being in those struggling with this painful condition.
Latest Updates and Emerging Research
Discover the latest insights into proctalgia fugax and its causes, as well as emerging treatments that may provide relief from this condition.
New insights into the condition
Recent developments in medical knowledge have been providing new insights into the condition of proctalgia fugax. Through high-resolution anorectal manometry, a technique designed to measure the pressure within the rectum, researchers are gaining real-time data and conclusions about this type of chronic anal pain disorder.
This information is also helping practitioners understand more about pelvic floor dysfunctions underlying this mysterious condition which may often have physiological causes.
Further, research suggests that one-time episodes are far more common than recurrent events associated with proctalgia fugax, which means that Chronic Proctalgia is no longer used as a term since research demonstrated that people can suffer from 1 or many episodes in their lives without being considered having ‘chronic’ symptoms.
Promising treatment developments
In recent years, a number of potential treatments and relief options for proctalgia fugax have emerged. One case study reported the use of Clostridium botulinum type A toxin to give an anal sphincter injection which was effective against proctalgia fugax in some cases.
Other studies suggest that relaxation techniques such as yoga or meditation may also be useful in reducing symptoms associated with proctalgia fugax. In addition, physical therapy has been proposed as a way to reduce muscle tension leading to partial alleviate of pain caused by proctalgia fugax.
The latest advancements demonstrate the potential we now possess when it comes to treating this mysterious condition and provide hope for future solutions that can bring long-term relief from its bothersome symptoms.
When to Seek Medical Attention
It is important to seek medical attention for rectal pain that does not resolve after a few minutes or recurs frequently.
Red flags and warning signs
Seek medical attention if experiencing sudden, severe pain, pain lasting longer than 20 minutes, if the presence of blood in the stool is present, or if there is an alteration to bowel movements.
Importance of proper diagnosis
Obtaining an accurate diagnosis is essential for those experiencing symptoms of proctalgia fugax. A misdiagnosis can lead to ineffective treatment and unnecessary procedures, so it’s important to consult with a healthcare professional immediately.
To begin the diagnostic process, doctors assess the severity and duration of symptoms before ruling out any organic causes of anorectal pain. This step is crucial in determining if proctalgia fugax is present or if further investigation into alternative conditions may be necessary.
If left unaddressed due to improper diagnosis or other factors, individuals with proctalgia fugax will suffer from severe rectal aches that are often difficult to manage without proper intervention by medical professionals.
Conclusion and Resources
Finally, it is important for those suffering from proctalgia fugax to remember that while the condition may be unpleasant and uncomfortable, there are resources available to help manage their symptoms, such as self-care measures, relaxation techniques, medications, and therapy.
Summary of key points
Proctalgia fugax is a condition characterized by sudden and severe anal pain that typically only lasts a few seconds or minutes. It can be triggered by physical activities such as sexual activity, stress, constipation, and defecation.
The pain can be described as a blunt knife being inserted into the rectum or lower anus area, and there is often no clear cause of the discomfort. Treatment options for proctalgia fugax involve lifestyle modifications (such as warm baths), medications (like calcium channel blockers and nitrates), relaxation techniques, and physical therapy; managing stress with appropriate therapies may also play an important role in reducing episodes of proctalgia fugax.
When experiencing any kind of sharp anal pain, it’s important to seek medical attention so that other causes of these symptoms can be ruled out.
Additional sources for information and support
- Online resources: Reading up on reliable sites such as the American Gastroenterological Association website can provide additional information about proctalgia fugax, including details of its diagnosis and management.
- Support groups: Joining an online or in-person support group with members who have similar experiences can be helpful for individuals seeking more information or support regarding proctalgia fugax.
- Healthcare professionals: Consulting healthcare professionals, such as a gastroenterologist, physical therapist, or mental health professional, is another way to obtain accurate information and learn of potential treatments.
Frequently Asked Questions (FAQs)
If you want to know more about proctalgia fugax, check the answers below.
1. What is Proctalgia Fugax?
Proctalgia Fugax is a medical condition characterized by brief, painful episodes of spasms in or around the anus.
2. Are there any risk factors associated with Proctalgia Fugax?
Certain factors may increase an individual’s risk of developing Proctalgia Fugax, such as prolonged sitting, excessive straining during defecation, and stress.
Note: Fixed typo error on prior sentence replacing “They” with “an individual.”
3. What are the symptoms associated with Proctalgia Fugax?
The primary symptom associated with Proctalgia Fugax is sudden and intense pain in the rectal area that resolves by itself within minutes without treatment. Other associated symptoms include tenderness and soreness when touching the swollen area around the anus.
4. What treatment options are available for Proctalgia Fugax?
Treatment options for pro ct al gia f ug ax focus on relieving discomfort through self-care measures such as hot baths, stretching exercises, biofeedback training, or medications, including muscle relaxants and/or topical creams containing lidocaine. In some cases, surgery may also be considered if other treatments have been unsuccessful.
Disclaimer: This content is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. This information is not comprehensive and should not be used to make health or well-being decisions. Consult a qualified healthcare professional with questions about a medical condition, treatment options, or health regimen. This website or the content should never replace professional medical advice.